Closed-Loop Systems in Pregnancy: Aggressive Settings for Better Outcomes
Jun 05, 2025
Managing type 1 diabetes during pregnancy is one of the most complex challenges for both moms and their care teams.
The stakes are high — from preventing congenital anomalies and preterm birth to reducing risks like preeclampsia and macrosomia. (1).
That’s why international guidelines set ultra-tight glucose targets: (2, 3)
✔️ HbA1c <6% (42 mmol/mol) at conception, or <7% (53 mmol/mol) if there is a risk of hypoglycemia
✔️ Fasting glucose <95 mg/dl (5.3 mmol/l)
✔️ Post-meal spikes tightly controlled: 1-hour postprandial glucose <140 mg/dL (7.8 mmol/l), and 2-hour postprandial glucose <120 mg/dl (6.7 mmol/l)
✔️ Pregnancy Time-in-Range (TIRp: 63-140 mg/dl or 3.5–7.8 mmol/l) >70% & Time-Below-Range (TBRp: <63 mg/dl or <3.5 mmol/l) <4%.
One study showed that even a 5% improvement in TIRp is linked to better maternal and neonatal outcomes. (4)
But here’s the reality — those targets are incredibly hard to hit.
👉 In early pregnancy, insulin needs drop, increasing the risk of lows.
👉 By the third trimester, insulin resistance rises rapidly, often doubling insulin needs by the end of the third trimester. (5)
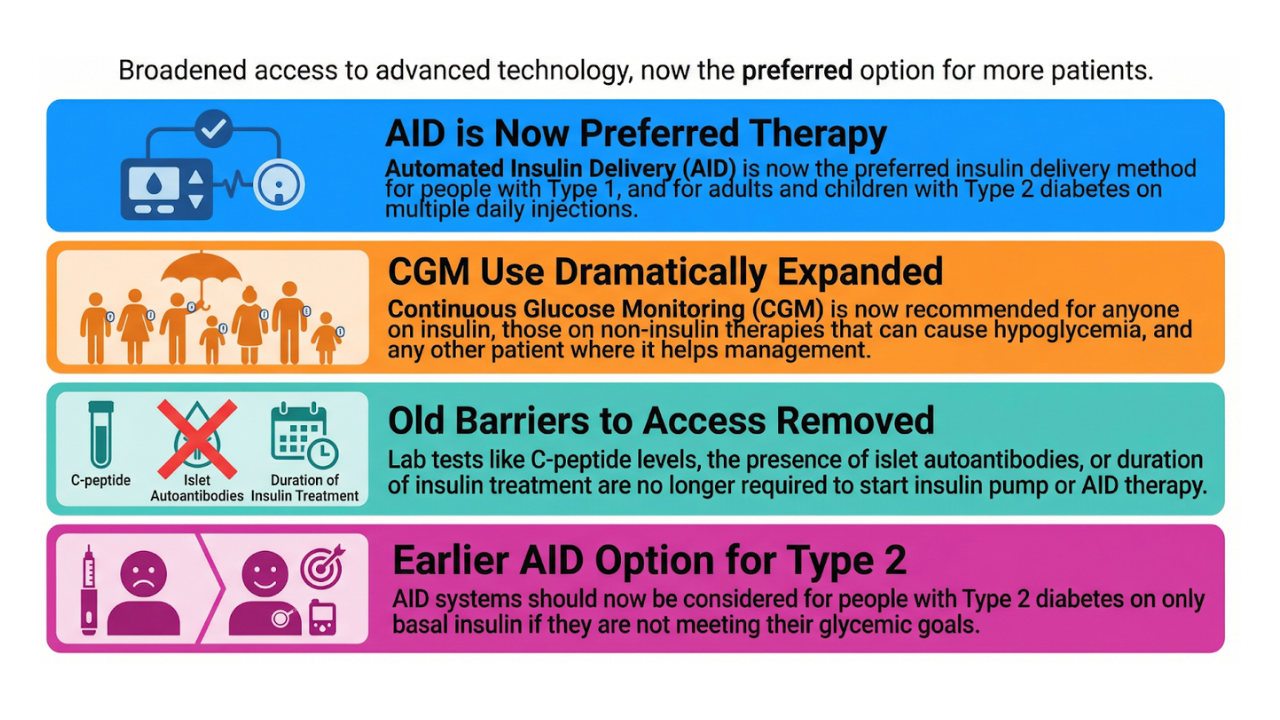
In recent years, the introduction of closed-loop systems has started a new era in the management of type 1 diabetes during pregnancy.
Large studies such as the AiDAPT trial (22) have shown that pregnant women using a closed-loop system can achieve a higher average TIRp (approximately 68%) than those on conventional therapy, without a higher risk of hypoglycemia or ketoacidosis.
However, the proportion of women who actually achieve >70% TIRp remains limited.
The targets therefore remain challenging, even with this technology.
Currently, only the CamAPS FX (mylife Loop) system is officially approved for use during pregnancy.
Other systems such as MiniMed 780G, Tandem Control-IQ, Omnipod 5, and various open-source closed-loop systems are used off-label, but also yield good results in practice.
The international ADA guideline (2) preferably recommends a system with pregnancy-specific targets (such as CamAPS FX), but other closed-loop systems can be considered - especially if you combine them with “assistive techniques” and have an experienced diabetes team supporting you.
In this blog we'll dive into assistive techniques and ways to tweak today’s closed-loop systems for maximum, aggressive, and safe glucose control.
This isn’t just for pregnant users—anyone wanting tighter glucose control with their closed-loop system might find useful tips here.
- We’ll start with general strategies for super-strict glucose control,
- then go through specific tweaks for different closed-loop systems,
- and finally discuss how to handle closed-loop systems during and after delivery.
Get Access To Updated Diabetes Technology Courses
General Guidelines for Achieving Very Strict Glucose Control with Closed-Loop Systems
See reference 6-14 below for related studies
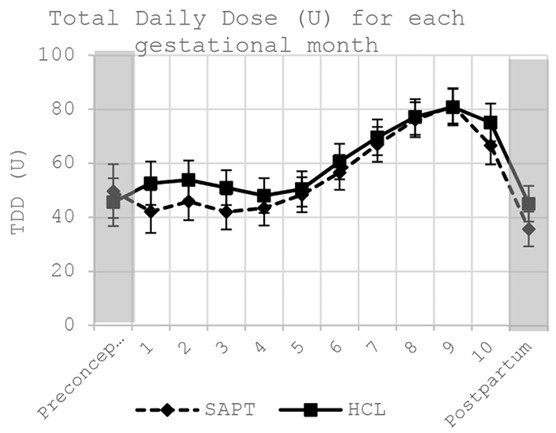
Figure 1: shows average rise in total daily insulin dose during pregnancy in 23 pregnant women with type 1 diabetes from the PICLS Study on sensor augmented pump therapy (SAPT) or hybrid closed-loop system (HCL) (5)
1. Optimise settings every 1-2 weeks
Pregnancy changes things fast, and your settings need to keep up. Here’s what to look at:
- Glucose target: Use the lowest target the system allows. Only a few systems—CamAPS FX, twiist, and open-source closed-loop systems—let you set targets that match the strict fasting goal for pregnancy (<95 mg/dL or <5.3 mmol/L). Other systems like the MiniMed 780G and DBLG1 can provide a very close target of 100 mg/dl or 5.5 mmol/l
- Temporary targets: Some systems allow even lower temporary targets. For example, CamAPS FX has a Boost function, and twiist offers a Pre-Meal Range option.
- Basal rates: Even though most closed-loop systems automate insulin delivery independent of the preset basal rates, it’s important to keep the preset basal rates up to date. This is a backup in case the system reverts to manual mode or limited mode (sensor warmup, sensor failures, connection problems etc).
- Carb ratio: Review and adjust the carb ratios every 1–2 weeks. Early in pregnancy, you may need to weaken the carb ratio (because you’re more sensitive to insulin), but as pregnancy progresses, you’ll need to strengthen it as insulin resistance builds. By week 20 and beyond, insulin needs can rise by about 5% each week. Carb ratios can get as tight as 1-3 g/unit, and total insulin use might double by the third trimester (see figure 1).
- Insulin sensitivity: Update if the closed-loop system uses it to adjust insulin delivery in auto mode (see figure 2). In that case, insulin sensitivity should be at least as strong as 1700 ÷ total daily insulin (for pumps in mg/dl) or 90 ÷ total daily insulin dose (for pumps in mmol/l).
- Duration of insulin action: Update if the closed-loop system uses it to adjust insulin delivery in auto mode (see figure 2).
- Hypoglycemia threshold: Set the lowest hypoglycemia threshold to align with the lower glucose values in pregnancy (see figure 2).
- Other settings: See below for brand-specific advice.
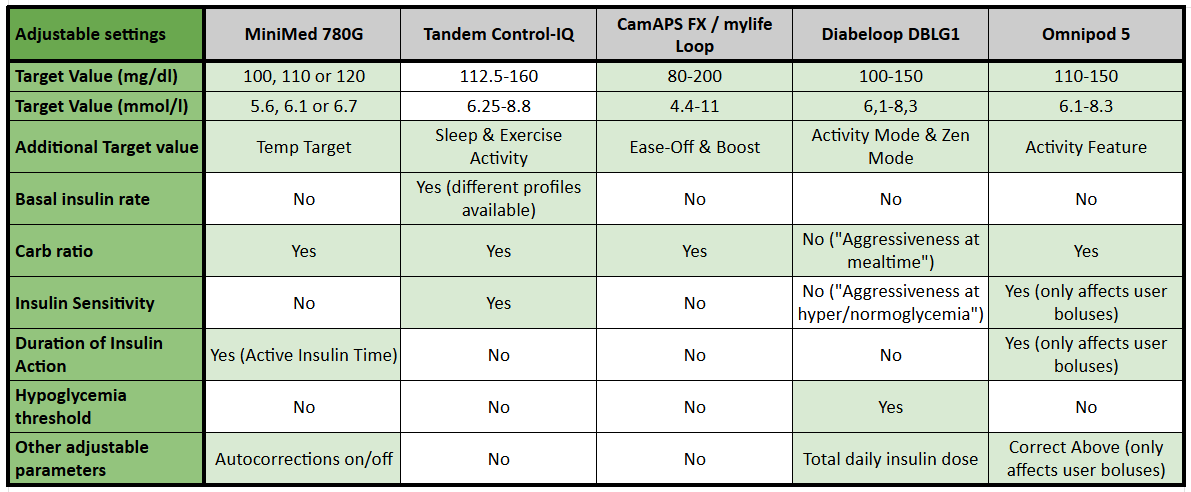
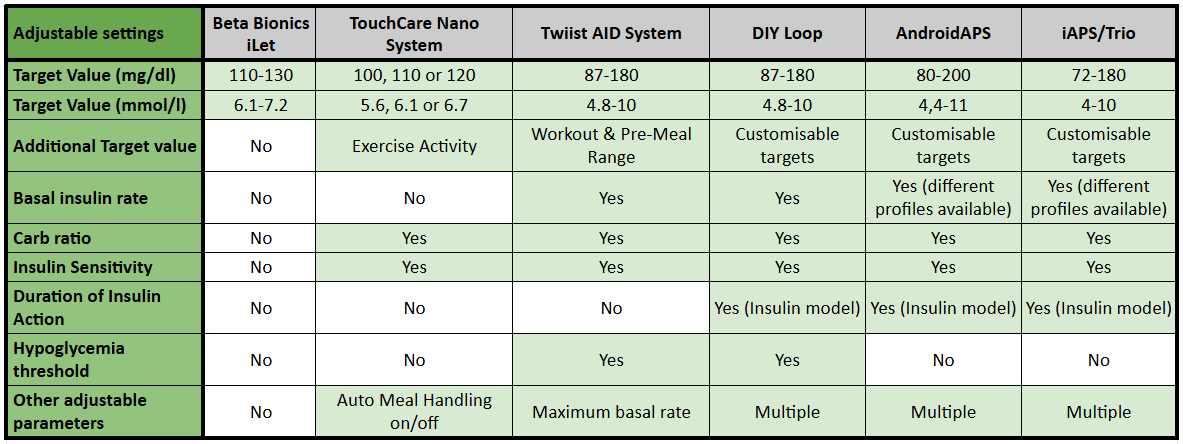
Figure 2: Overview of adjustable settings in 11 different closed-loop systems
2. Dial in your diet
Strict glucose control is mostly about what you eat. Think of it as 90% diet, 10% insulin.
- Choose foods with a low glycemic index (high in fiber, low in processed carbs)
- Be as accurate as possible with carb counting. Consider keeping a food diary, or using the “event” section in your app.
- Avoid very high-carb meals to prevent post-meal spikes, especially in the third trimester.
- Outside of pregnancy, some people do well with low-carb eating. But during pregnancy, it’s recommended to eat at least 175 grams of carbs per day for the baby’s brain and to avoid ketones (6). A possible pattern: 20 grams at breakfast, 40-60 grams at lunch/dinner, and 10-20 grams for snacks, as suggested by DTN-UK.
3. Bolus before eating
- In early pregnancy, premeal insulin should be given about 15 minutes before carbohydrate intake. As pregnancy advances, particularly in the third trimester, the optimal timing may extend to 30–40 minutes before eating—this is often especially important at breakfast.
- If the optimal pre-bolus timing is not known, one can bolus and watch for glucose levels to start to decrease on CGM before eating.
- For meals high in fat, split bolusing is recommended (unless the closed-loop system offers an extended bolus option) to better match insulin delivery to the meal’s absorption profile.
4. Correct highs fast and efficient
- Set a clear threshold and high alert for when to correct (for example > 160 mg/dL or 8.9 mmol/L).
- Correct with the bolus calculator, or use features like Boost.
- Sometimes it will be necessary to “override” the system by giving a manual bolus or entering “fake carbs.” Try not to do this more than once every 2 hours to avoid insulin stacking. (Note that this advice applies specifically during pregnancy. Outside of pregnancy, frequent intervention - such as giving extra boluses or fake carbs - can interfere with the learning process of the closed-loop system, making it less able to adapt to your increased insulin needs.)
5. Avoid over-treating lows
- Start with 5–10 grams of carbs (the system will suspend insulin delivery before a low anyway).
- Use a fingerstick to confirm hypoglycemia before treating a second time.
- Remember, in pregnancy the recommended lower threshold is 63 mg/dL (3.5 mmol/L), not 70 mg/dL (3.9 mmol/L).
6. Watch out for long basal suspensions
- If the pump suspends insulin for an hour or more, this can lead to rebound highs later.
- Check the pump reports for how often this is happening.
- If possible, tweak the settings to reduce these long suspensions.
7. Use manual mode if needed (for closed-loop systems without pregnancy-specific glucose targets)
- If the average glucose is running high overnight, consider switching to manual mode at night and turning auto mode back on in the morning.
- If you do this, make sure the low-glucose suspend feature is on, if this is available.
Fine-tuning settings and staying actively involved with the closed-loop system can lead to stricter glucose control and better pregnancy outcomes.
Many of these tips are also useful for anyone who wants tighter glucose control, even outside of pregnancy.
Device-Specific Guidelines for Achieving Strict Glucose Control with Closed-Loop Systems
See reference 17-39 below for related studies
Please note that, except for CamAPS FX (which is approved for use in pregnancy), closed-loop systems are not officially indicated for pregnancy.
The information below is not medical advice—always consult with a healthcare provider before making any changes to therapy.
1. CamAPS FX (mylife Loop)

- Glucose targets: 1st trimester: 100 mg/dL (5.6 mmol/L); 2nd & 3rd trimester: 80 mg/dL (4.4 mmol/L) overnight, 90 mg/dL (5.0 mmol/L) during the day
- Use Boost and Ease-Off more liberally than outside of pregnancy.
- Update weight every 2–4 weeks.
- Basal rates: Update using a percentage of the total daily dose, not the actual basal delivered.
- More information: See the official CamAPS FX pregnancy leaflet.
Intra/postpartum:
- Glucose target: 100–110 mg/dL (5.6–6.1 mmol/L) at the start of labor or fasting for caesarean.
- For hypoglycemia trend: Use Ease-Off or a higher target.
- Prepare a postpartum profile (basal rates, carb ratio) and enter these settings into the CamAPS FX app after delivery
- Update to postpartum weight.
2. MiniMed 780G

- Glucose target: 100 mg/dL (5.5 mmol/L)
- Active insulin time: 2 hours
- If "Safe Meal Bolus" occurs frequently and results in postprandial hyperglycemia, when strengthening the carb ratio, then relax the carb ratio and add extra “fake carbs” with meals (for example 20-100% extra carbs).
Intra/postpartum:
- Glucose target: 100–110 mg/dL (5.6–6.1 mmol/L) at the start of labor or fasting for caesarean.
- For hypoglycemia trend: Use Temp Target or increase target.
- Prepare a postpartum profile (basal rates, carb ratio) and enter these settings into the MiniMed pump after delivery.
3. Tandem with Control-IQ technology

- Use Sleep Mode 24/7 (day and night).
- Programmed basal rates should be 20–25% higher than actual delivered basal, but avoid excessive high basal rates to prevent rebound hyperglycemia (Control-IQ reduces/suspends basal insulin when predicted glucose is below 112.5 mg/dL (6.3 mmol/L) or 70 mg/dL (3.9 mmol/L), respectively).
- Do not accept recommended bolus reduction if glucose is <110 mg/dL (6.1 mmol/L).
- Use the “super bolus technique” if persistent postprandial hyperglycemia: turn Control-IQ temporarily off during meals, reduce basal insulin delivery for 2–3 hours after a meal and add this amount to the mealtime bolus, either as extra carb bolus or correction. This approach delivers more insulin up front while minimizing postprandial basal insulin, which can help manage post-meal glucose spikes.
- Update total insulin dose and weight every 4 weeks.
Intra/postpartum:
- Switch to regular Control-IQ (not Sleep Mode) at the start of labor or fasting for caesarean.
- For hypoglycemia trend: Use Activity Mode.
- Preset a postpartum profile in the insulin pump (basal rates, carb ratio, correction factor) and switch to this profile after delivery.
- Update to postpartum weight and total insulin dose.
4. Omnipod 5

- Use the lowest glucose target (110 mg/dL or 6.1 mmol/L).
- Use the lowest "correct above" target (110 mg/dL or 6.1 mmol/L) and duration of insulin action (2 hours).
- Turn off “Reverse Correction.”
Intra/postpartum:
- For hypoglycemia trend: Use Activity Feature or a higher glucose target.
- After delivery, consider a hard reset of the algorithm. This will erase all settings, adaptive basal rates, and history. After the reset, restart the Omnipod 5 system using the prepregnancy settings (basal rate, carb ratio, insulin sensitivity, etc.). The Omnipod 5 system will estimate a new total daily insuln dose based on the reduced Basal Program (from Manual Mode) and set a new (weaker) Adaptive Basal Rate.
5. DBLG-1 (Diabeloop)

- Use the lowest glucose target (100 mg/dL or 5.6 mmol/L).
- Increase total daily insulin and aggressiveness (at hyperglycemia, normoglycemia and meals) every 1–2 weeks after week 12 as needed.
Intra/postpartum:
- For hypoglycemia trend: Use Physical Activity Feature or a higher glucose target.
- Prepare a postpartum profile (basal rates, total daily insulin dose) and enter these settings into the DBLG1 handset after delivery + reset all aggressiveness factors to 100%.
6. iLet (Beta Bionics)

- Use the “lower” glucose target (110 mg/dL or 6.1 mmol/L).
- Update weight every 2–4 weeks.
Intra/postpartum:
- Use the “higher” glucose target (130 mg/dL or 7.2 mmol/L) at the start of labor or fasting for caesarean.
Note: iLet is less aggressive than other closed-loop systems and is generally not preferred in pregnancy.
7. AndroidAPS

- Glucose targets: 1st trimester: 100 mg/dL (5.5 mmol/L); 2nd & 3rd trimester: 80 mg/dL (4.4 mmol/L) overnight, 90 mg/dL (5.0 mmol/L) during the day
- Set patient type to "pregnant" for more aggressive insulin delivery. The algorithm will automatically adjust several limits.
- (Join the DIY Looping and Pregnancy Facebook group)
Intra/postpartum:
- Glucose target: 100–110 mg/dL (5.6–6.1 mmol/L) at the start of labor or fasting for caesarean.
- For hypoglycemia trend: Use a higher target or lower insulin percentage.
- Preset a postpartum profile in the AndroidAPS app (basal rates, carb ratio, correction factor) and switch to this profile after delivery.
8. DIY Loop / twiist Loop

- Use the lowest glucose target: 1st trimester: 100 mg/dL (5.5 mmol/L); 2nd & 3rd trimester: 87 mg/dL (4.8 mmol/L).
- Set the lowest Glucose Safety Limit (67 mg/dL or 3.7 mmol/L).
- Use Pre-Meal target before meals, but premeal bolusing is preferred for post-meal spikes.
- Recommended bolus types: For breakfast, use a Lollipop (2h) bolus; for later meals with more fat, use Taco (3h) or Pizza (4h) boluses.
- (Join the DIY Looping and Pregnancy Facebook group)
Intra/postpartum:
- Glucose target: 100–110 mg/dL (5.6–6.1 mmol/L) at the start of labor or fasting for caesarean.
- For hypoglycemia trend: Use a higher glucose target or lower insulin percentage (Workout Range in twiist).
- Prepare a postpartum profile (basal rates, carb ratio, insulin sensitivity) and enter these settings into the Loop app after delivery.
Pro tip: Using Other Insulins
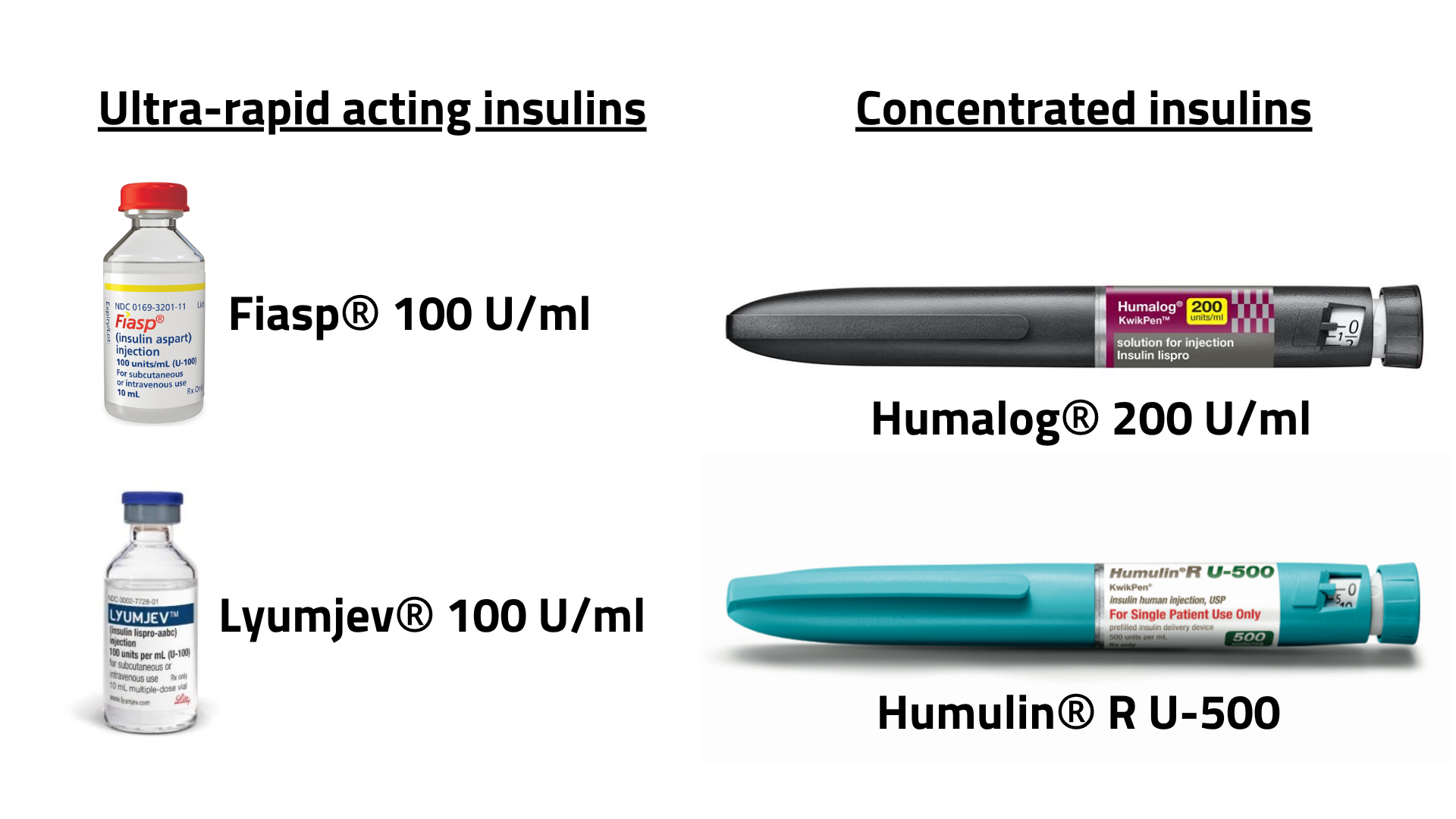
Ultra-rapid insulins
Most studies report that ultra-rapid insulins improve postprandial glucose control, yet they do not significantly increase overall Time in Range (40-44).
One trial also found a higher rate of unplanned infusion‐set changes with these formulations (45).
Fiasp® and Lyumjev® are both approved for use in pregnancy and lactation; however, not every insulin pump or closed‐loop system has been tested or labeled for use with these ultra-rapid acting insulins. To date, there are no published studies examining Fiasp® or Lyumjev® within closed-loop systems during pregnancy.
Concentrated insulins (off-label)
During pregnancy, insulin requirements often double. Some pumps have limited reservoir or patch capacity (usually 180–300 units per reservoir), which means frequent renewels may be needed.
To reduce the need for daily or twice-daily changes, some people use concentrated insulin in their pumps (off-label).
Here's how to do this for U200 insulin lispro (Humalog® 200):
- Multiply carb ratio and insulin sensitivity by 2
- Divide basal rates by 2
- Insulin action time remains the same as U100
Here's how to do this for U500 regular insulin (Humulin® R U500):
- Multiply carb ratio and insulin sensitivity by 5
- Divide basal rates by 5
- Use a longer insulin action time (at least 5 hours)
If switching insulin concentration in a pump with a learning algorithm (like Omnipod 5), consider resetting the algorithm, using a higher glucose target, or switching to manual mode for a few days to allow the system to adapt safely.
Intra/postpartum
See reference 44-49 below for related studies
Labor and Delivery
Tight glucose control during labor and delivery is linked to lower rates of neonatal hypoglycemia. Glucose targets during this time vary by professional society, but most recommend keeping glucose between 70 and 126 mg/dL (3.9–7.0 mmol/L).
Using insulin pumps—including closed-loop systems—often achieves better glucose control than switching to intravenous (IV) insulin (46). Recent data with the MiniMed 780G system during delivery have been positive (48). The potential use of a closed-loop system during labor should be discussed with all parties involved (the person with diabetes, the diabetes care team, the obstetric team, and the anesthesiologist).
Suggested Instructions for Continuing Closed-Loop Systems During Labor and Delivery
- The current insulin infusion site should be less than 24 hours old and placed away from the central abdomen or suprapubic area (important if a cesarean section may be needed).
- Bring extra pump supplies (cartridges, reservoirs, infusion sets, pods) and a backup CGM sensor to the hospital.
- If glucose rises above 110 mg/dL (6.1 mmol/L), a correction dose can be given.
- If glucose falls below 70 mg/dL (3.9 mmol/L), give 8–10 g of oral carbohydrate if eating is allowed, or IV dextrose if not. Consider increasing the glucose target if hypoglycemia is a concern.
- Switch to the postpartum profile at the time of delivery.
- If the person in labor cannot manage the pump due to complications or ongoing low/high glucose, discontinue pump therapy and switch to IV insulin following hospital protocols. When using IV insulin, blood glucose monitoring must be done with fingersticks to guide insulin adjustments, but CGM can still be used as an extra tool.
Postpartum & Breastfeeding
- Adjust settings on the closed-loop system to prepregnancy settings as soon as possible after delivery. Insulin doses usually need to be reduced by about 50% compared to late third trimester requirements, to lower the risk of hypoglycemia. Some experts recommend using a dedicated postpartum profile with insulin delivery set lower than pre-pregnancy settings—for example, basal rates at about two-thirds, carbohydrate ratios 10–20% less aggressive, and insulin sensitivity 20% reduced (11). The exact reduction should be individualized for each person.
- Special care is needed with the first postpartum meal bolus, as insulin resistance drops quickly and there is a higher risk for hypoglycemia.
- Breastfeeding increases the risk of hypoglycemia, especially overnight. Consider reducing basal rates (Tandem t:slim X2 with Control-IQ) or using higher glucose targets or activity mode during breastfeeding (all closed-loop systems).
Conclusion
Closed-loop systems are now recommended for managing type 1 diabetes during pregnancy, labor, and delivery. These systems improve glucose control and reduce hypoglycemia, but reaching the strict targets—especially a pregnancy Time in Range (TIRp) above 70%—remains challenging, even for well-supported patients.
Although CamAPS FX (myLife Loop) is currently the only closed-loop system officially approved for use during pregnancy, both commercial and open-source closed-loop platforms can offer valuable benefits when deployed thoughtfully and with adequate support.
Closed-loop systems allow more responsive, adaptive insulin delivery in the face of rapidly changing needs during pregnancy, labor, and postpartum. Alongside the technology, success also depends on attention to basics: accurate carb counting, careful pre-bolusing, and regular setting adjustments as insulin needs change through each trimester and after delivery.
Still, there are barriers—including lack of pregnancy-specific algorithms, regulatory limitations for many devices, and the ongoing need for clinician and user education. Ongoing research, better access, and continuous education for both healthcare professionals and people living with diabetes will be essential to make these benefits available to all who need them.
Closed-loop therapy is quickly becoming the new standard of care for pregnancy in type 1 diabetes. With the right support, it has the potential to transform outcomes for mothers and babies alike.
Want to learn more?
Don’t miss Diana Isaacs’ outstanding presentation from the 2024 Diabetes Technology Conference, available as a free webinar via danatech from ADCES. The session is accredited for US healthcare providers and provides a practical, in-depth overview of closed-loop therapy in pregnancy.
Watch the danatech webinar from ADCES here.
Good luck,

Related studies
General
- 1 Ringholm et al. Improving pregnancy outcomes in women with diabetes mellitus: modern management. Nat Rev Endocrinol 2019.
- 2 ElSayed et al. Management of Diabetes in Pregnancy: Standards of Care in Diabetes—2025. Diabetes Care 2025
- 3 Battelino et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care 2019
- 4 Murphy et al. CGM in type 1 diabtes pregnancy: every 5% Time in range matters. Diabetologia 2019
- 5 King et al. Changes to insulin pump settings throughout pregnancy for individuals using assisted hybrid closed-loop therapy versus sensor-augmented pump therapy. J Diabetes Complications Apr 2025
- 6 Benhalima et al. Management of type 1 diabetes in pregnancy: update on lifestyle, pharmacological treatment, and novel technologies for achieving glycaemic targets. Lancet Diabetes Endocrinol 2023 - Benhalima et al. Automated Insulin Delivery in Pregnancies Complicated by Type 1 Diabetes. JDST Mar 2025
- 7 Szmuilowicz et al. Expert Guidance on Off-Label Use of Hybrid Closed-Loop Therapy in Pregnancies Complicated by Diabetes. DTT 2023
- 8 Quiros et al. Real-world prospective cohort study comparing closed-loop therapy (n=59) with MDI (n=53) in pregnant women with type 1 diabetes. DTT Aug 2024
- 9 Sobhani et al. Review of observational trials of closed-loop systems in pregnant women with type 1 diabetes. JDST Mar 2025
- 10 Scifres et al. Expert guidance on use of closed-loop therapy in pregnancies complicated by diabetes. JDST April 2025
- 11 Szmuilowicz et al. Expert guidance on use of CGM and closed-loop therapy in pregnancies complicated by diabetes. JDST May 2025
- 12 Hand et al. Expert guidance on off-label use of hybrid closed-loop therapy in pregnancies complicated by diabetes. JDST May 2025
- 13 Jones et al. Real-world observational analysis of CGM metrics pre- and post closed-loop therapy in n=43 pregnant women with type 1 diabetes. JDST May 2025
- 14 Tahir et al. Hybrid closed loop insulin therapy versus standard therapy in pregnant women with type 1 diabetes: A systematic review and meta-analysis of randomized controlled trials.
CamAPS FX
-
18 Stewart et al. Closed-Loop Insulin Delivery during Pregnancy in Women with Type 1 Diabetes. NEJM 2016
-
19 Steward et al. Day-and-Night Closed-Loop Insulin Delivery in a Broad Population of Pregnant Women With Type 1 Diabetes: A Randomized Controlled Crossover Trial. Diabetes Care 2018
-
20 Steward et al. Adaptability of Closed Loop During Labor, Delivery, and Postpartum: A Secondary Analysis of Data from Two Randomized Crossover Trials in Type 1 Diabetes Pregnancy. DTT 2018
-
21 Rankin et al. Rollout of Closed-Loop Technology to Pregnant Women with Type 1 Diabetes: Healthcare Professionals' Views About Potential Challenges and Solutions. DTT 2023
-
22 AiDAPT study. Automated Insulin Delivery in Women with Pregnancy Complicated by Type 1 Diabetes. NEJM 2023
MiniMed 780G
Tandem Control-IQ
Omnipod 5
Diabeloop
AndroidAPS
- 33 Schütz-Fuhrmann et al. Two Subsequent Pregnancies in a Woman With Type 1 Diabetes: Artificial Pancreas Was a Gamechanger
JDST 2020 - 34 Lemieux et al. Do-It-Yourself Artificial Pancreas System Use in Pregnant Women With Type 1 Diabetes in a Real-World Setting: 2 Case Reports. Canadian Journal of Diabetes 2021
- 36 Sobhani et al. Use of Open-Source Automated Insulin Delivery Systems in Pregnancies With Type 1 Diabetes. JDST 2023
- 37 Hawke et al. Supported Open-Source Automated Insulin Delivery for Management of Type 1 Diabetes in Pregnancy. JDST May 2025
DIY Loop
Insulins
- 40 Dutta et al. Performance of Fast-Acting Aspart Insulin as Compared to Aspart Insulin in Insulin Pump for Managing Type 1 Diabetes Mellitus: A Meta-Analysis. Diabetes Meta J 2023
- 41 Dovc et al. Postprandial time in tight range with faster insulin aspart compared with standard insulin aspart in youth with type 1 diabetes using automated insulin delivery. Diabetes Obes Metab 2025
- 42 Levy et al. Multicenter Evaluation of Ultra-Rapid Lispro Insulin with Control-IQ Technology in Adults, Adolescents, and Children with Type 1 Diabetes. DTT 2024
- 43 Haliloglu et al. Postprandial Glucose Excursions with Ultra-Rapid Insulin Analogs in Hybrid Closed-Loop Therapy for Adults with Type 1 Diabetes. DTT 2024
- 44 Stamati et al. Efficacy and safety of ultra-rapid insulin analogues in insulin pumps in patients with Type 1 Diabetes Mellitus: A systematic review and meta-analysis. Diabetes Res Clin Pract 2022