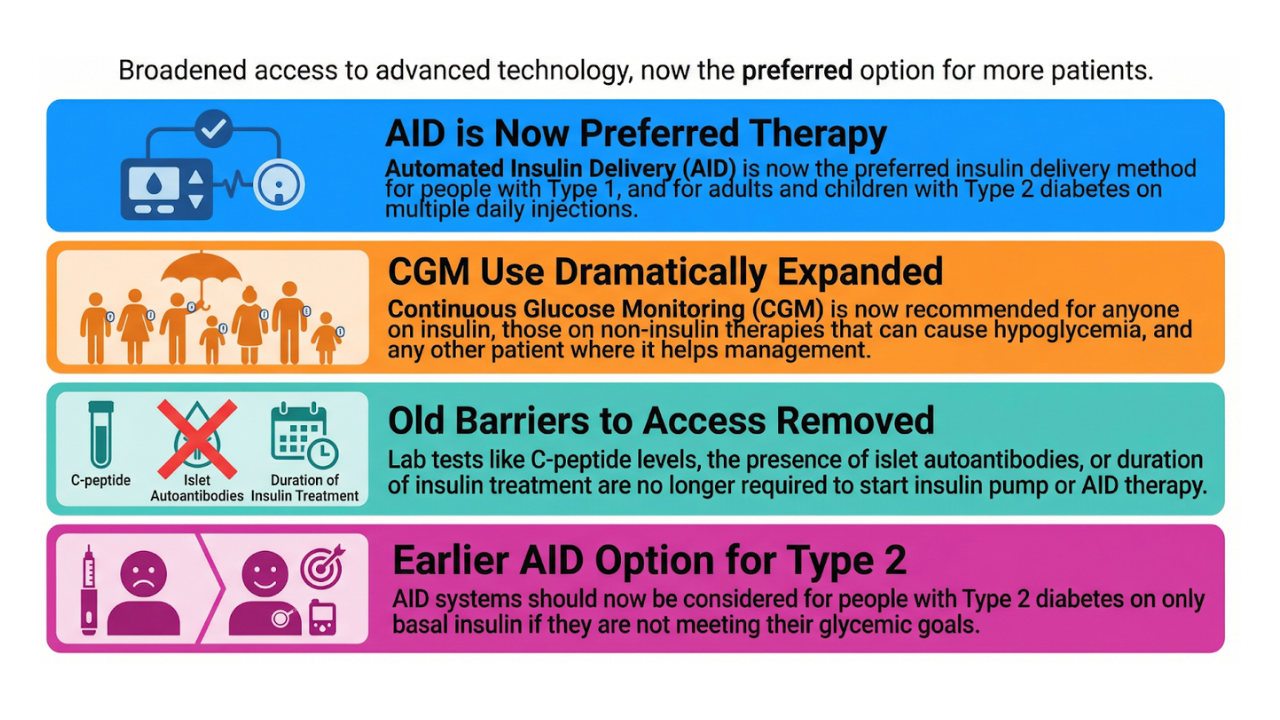
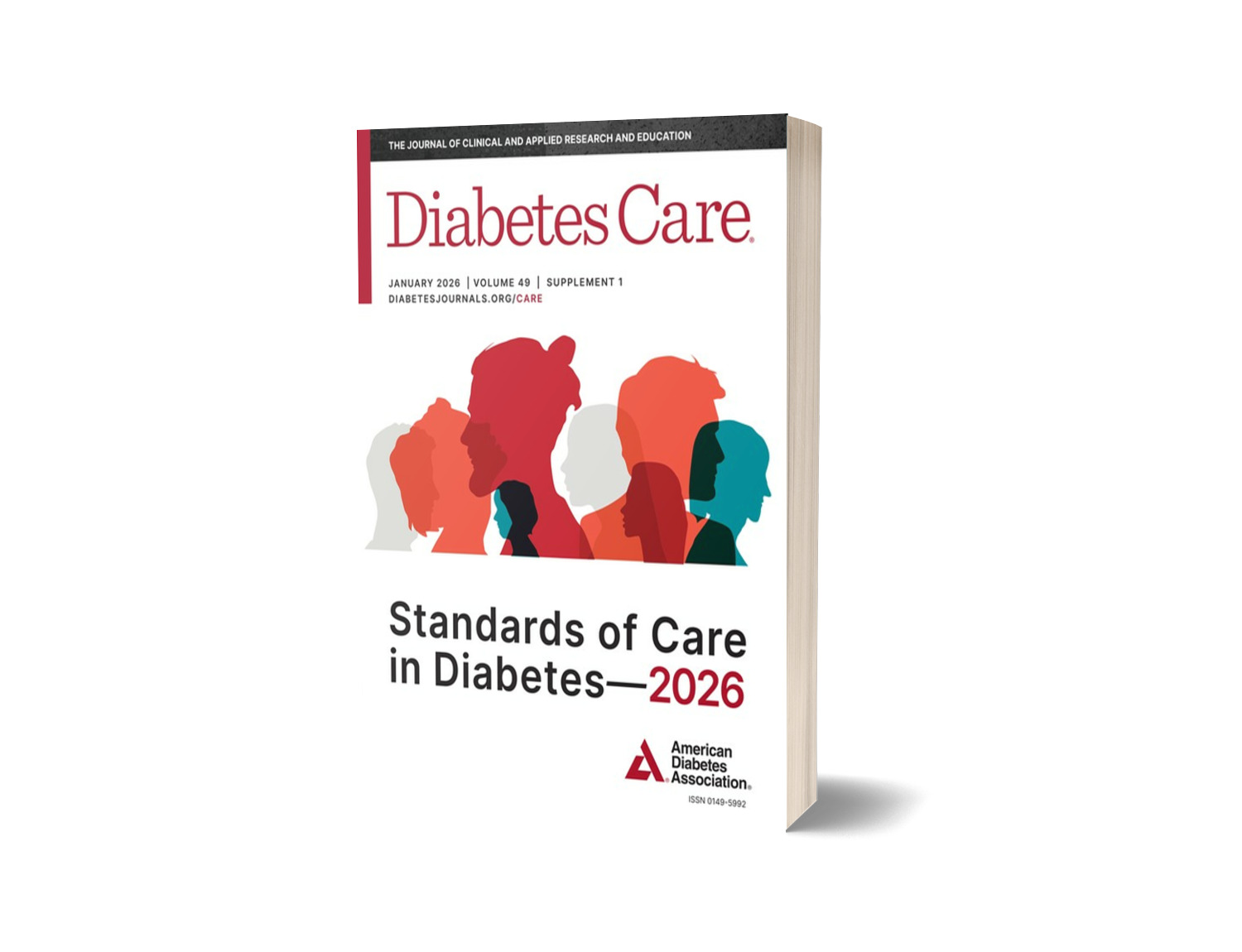
Key Updates: ADA 2026 Diabetes Technology Guidelines
Dec 12, 2025
The American Diabetes Association has released the Standards of Care in Diabetes—2026, and this year’s technology section doesn’t tiptoe around progress. It accelerates it.
The theme is unmistakable: earlier access, fewer barriers, and more trust in both automation and the people who use it.
If you work with diabetes technology—or live with diabetes—these changes matter.
Below is a clear breakdown of the most important updates in Section 7 (Diabetes Technology),
focusing on CGM, automated insulin delivery, and open-source tools.
Get Access To Updated Diabetes Technology Courses
1. CGM for Far More People
What you measure, you can improve—and now more people get to measure.
|
Recommendation 7.15 |
Use of CGM is recommended at diabetes onset and anytime thereafter for children, adolescents, and adults with diabetes who are on insulin therapy, A on noninsulin therapies that can cause hypoglycemia, C and on any diabetes treatment where CGM helps in management. C The specific CGM device and method for use should be made based on the individual’s circumstances, preferences, and needs. E |
|
Recommendation 7.8 |
Consider early initiation, including at diagnosis, of CGM, CSII, and AID depending on a person’s or caregiver’s needs and preferences. C |
What Changed?
- Broader eligibility: People with type 2 diabetes on non-insulin therapies are explicitly included when CGM helps with glucose management.
- Earlier access: CGM at diagnosis is encouraged. No need to “wait until things get worse”.
- OTC (Over The Counter) CGMs acknowledged: Useful for people with prediabetes or type 2 diabetes wanting lifestyle feedback.
- Emphasis on preferences: Technology should serve the person—not the other way around.
Reality Check
No, it’s not “CGM for absolutely everyone regardless of context.”
Yes, it is a major broadening.
The ADA is clearly saying: If CGM can help—and the person wants it—offer it. Early.
2. AID Systems Become the Preferred Insulin Delivery Method
Automation isn’t the future. It’s the baseline.
|
Recommendation 7.25a |
AID systems are the preferred insulin delivery method over MDI, CSII, and sensor-augmented pumps in people with type 1 diabetes, A adults with type 2 diabetes, A children and adolescents with type 2 diabetes, E and those with other forms of insulin-deficient diabetes. B, C, D, E Choice of an AID system should be made based on the individual’s circumstances, preferences, and needs. E |
|
Recommendation 7.25b |
Consider AID systems for select people with type 2 diabetes treated with basal insulin not achieving individualized glycemic goals. B Choice of an AID system should be made basedon the individual’s circumstances, preferences, and needs. E |
|
Recommendation 7.8 |
Consider early initiation, including at diagnosis, of CGM, CSII, and AID depending on a person’s or caregiver’s needs and preferences. C |
What Changed?
- Preferred method: AID (Automated Insulin Delivery) is positioned above MDI (Multiple Daily Injections) and pump therapy without automation.
- Barrier removal: No more C-peptide minimum, auto-antibody requirements, or “6–12 months on insulin first”.
- Earlier adoption: AID can be offered as soon as someone is ready for it—even at diagnosis.
- Expanded eligibility: AID can also be considered for people on basal-insulin–only therapy who are not achieving individualized glycemic goals.
Reality Check
AID is the preferred method, not mandated.
Support, readiness, and individual context still guide the choice.
But the hierarchy is clear:
If you’re using insulin intensively, AID is now the ADA default recommendation.
3. Recognition of Open-Source AID and Digital Health Tools
Innovation doesn’t only come from industry. Sometimes the community leads.
|
Recommendation 7.27 |
Support and provide diabetes management advice to people with diabetes who choose to use an open-source AID system. B |
|
Recommendation 7.28 |
Consider combining technology (CGM, insulin pump, and/or diabetes apps) with online or virtual licensed coaching to improve glycemic outcomes in individuals with diabetes or prediabetes. B |
What Changed?
- Open-source AID is officially recognized—again, and more strongly. Systems such as AndroidAPS, Loop, iAPS, and Trio are explicitly included.
- Digital coaching endorsed: Apps + sensors + telehealth = better outcomes.
This is one of the clearest acknowledgements yet that patient-driven tech is part of mainstream diabetes care—and that clinicians should engage, not avoid.
4. Continue Using CGM and AID During Hospitalization
If a person manages their diabetes well at home, don’t disable their tools in the hospital.
|
Recommendation 7.29 |
In people with diabetes wearing personal CGM, the use of CGM should be continued when clinically appropriate during hospitalization, with confirmatory point-of-care glucose measurements for insulin dosing and hypoglycemia assessment and treatment under an institutional protocol. B |
|
Recommendation 7.30 |
Continue use of insulin pump or AID in people with diabetes who are hospitalized when clinically appropriate. This is contingent upon availability of necessary supplies, resources, training, ongoing competency assessments, and implementation of institutional diabetes technology protocols. C |
What Changed?
- Stronger wording
- Clear expectations for institutional protocols
- Reinforcement that device continuity is safer when managed correctly
Hospitals need workflows—not excuses.
Why This Matters
The ADA Standards shape policy, reimbursement, access, and daily clinical practice.
This year’s message is loud and clear:
- Technology should be available early, not as a last resort.
- People with diabetes should have more agency, not more hoops.
- Automation, digital tools, and open-source solutions deserve clinical support, not silence.
- Hospitals must modernize—not default to disconnecting devices.
Or as one systems thinker put it:
“The future is already here. It’s just not evenly distributed.”
The ADA is trying to fix that distribution.
Want to Go Deeper? Explore Our Free Diabetes Tech Courses
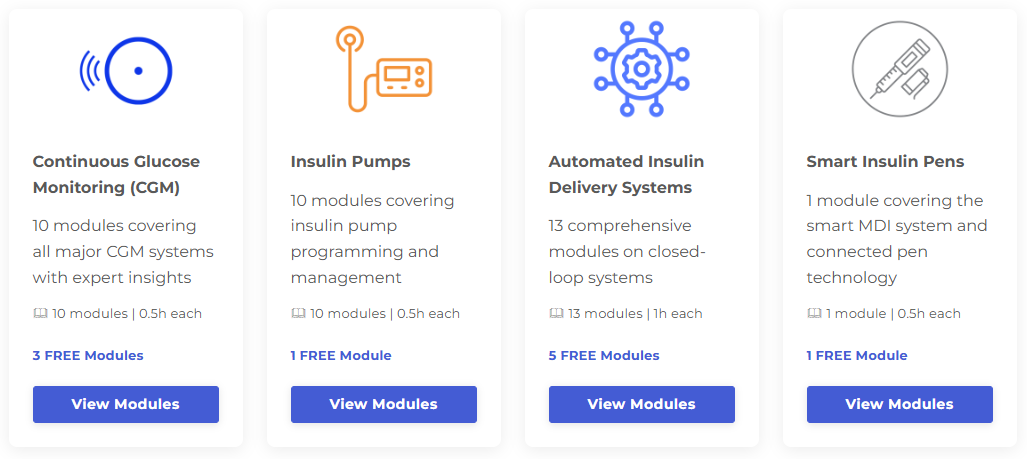
At Diabetotech, we make advanced diabetes technology clear, practical, unbiased, and accessible—for clinicians, educators, and people with diabetes.
You can now access free courses on:
- Continuous glucose monitoring
- Insulin pumps
- Automated insulin delivery systems
- All major open-source AID systems
Fresh updates this week:
- The AndroidAPS module is fully updated
- The DIY Loop module has been refreshed
- iAPS will be updated right after Christmas
- A brand-new, free module on Trio is now live
Each module is peer-reviewed and built for real-world use—not marketing.
Explore the free modules:
If you want to stay ahead of the curve, this is the place to start.
Kind regards,

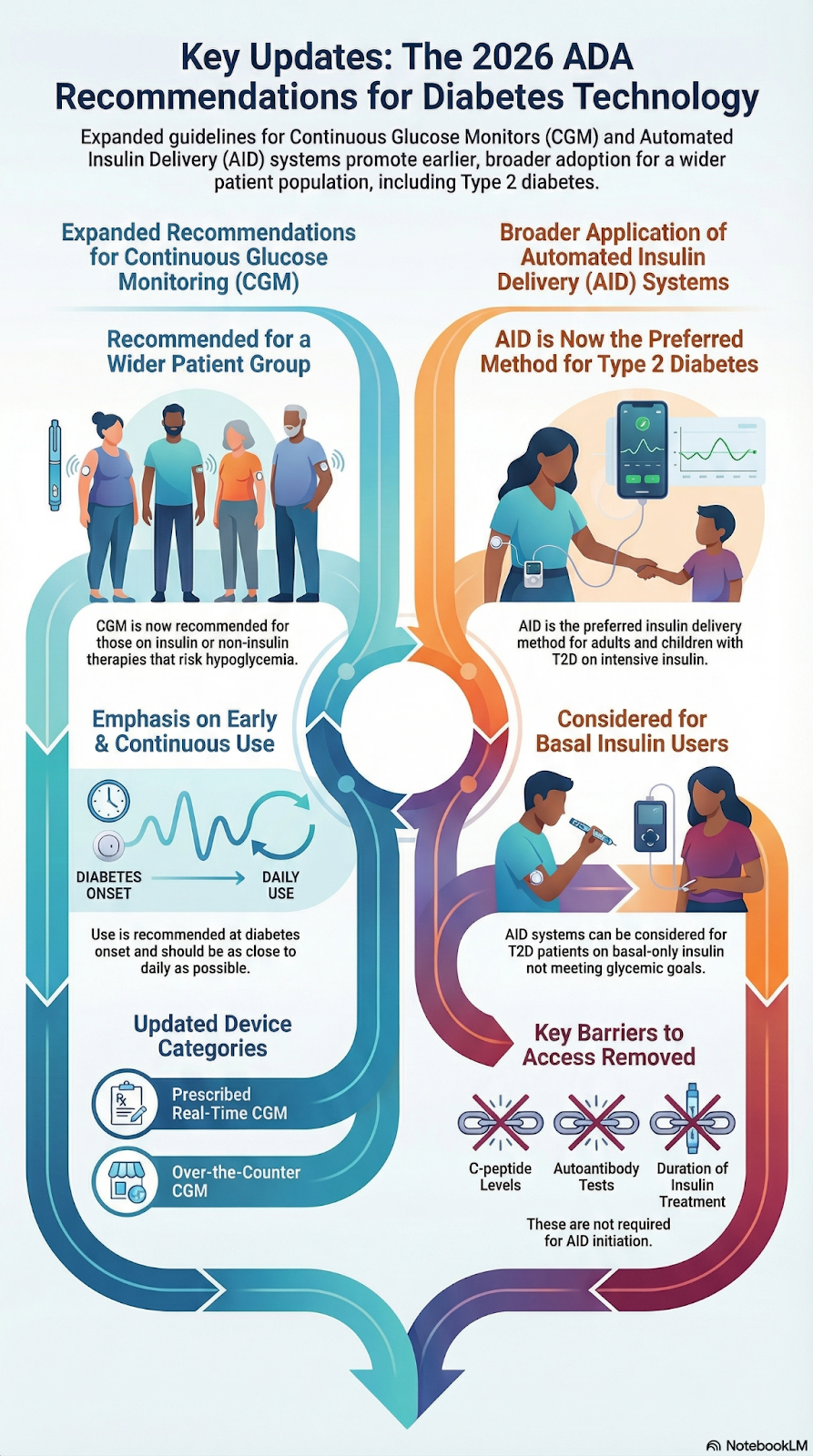
Infographic made with NotebookLM based on Section 7 of ADA guidelines 2026 compared to 2025