CES 2026: When Diabetes Technology Becomes Consumer Technology
Jan 15, 2026
CES is the world’s largest consumer electronics show. Early January. Las Vegas.
This year: 148,000+ attendees, 4,100 exhibitors, and a familiar atmosphere of optimism where technology is always about to change everything.
For healthcare professionals, CES is not about gadgets. It’s about the direction of travel.
And CES 2026 made one thing unmistakably clear:
Diabetes technology—especially CGM—is no longer positioning itself as medical infrastructure.
It is positioning itself as consumer intelligence.
That shift has consequences for clinical care, expectations, and our role as professionals.
Diabetes technology has crossed the consumer Rubicon
![]()
For the first time, diabetes technology was not a niche presence at CES.
It was embedded in the broader biowearables and lifestyle health narrative.
Independent reviewers picked this up immediately. The framing was telling: not disease management, but performance, awareness, and optimisation.
Glucose was no longer discussed as a pathology marker.
It was presented as a feedback signal you can learn from.
That reframing has consequences.
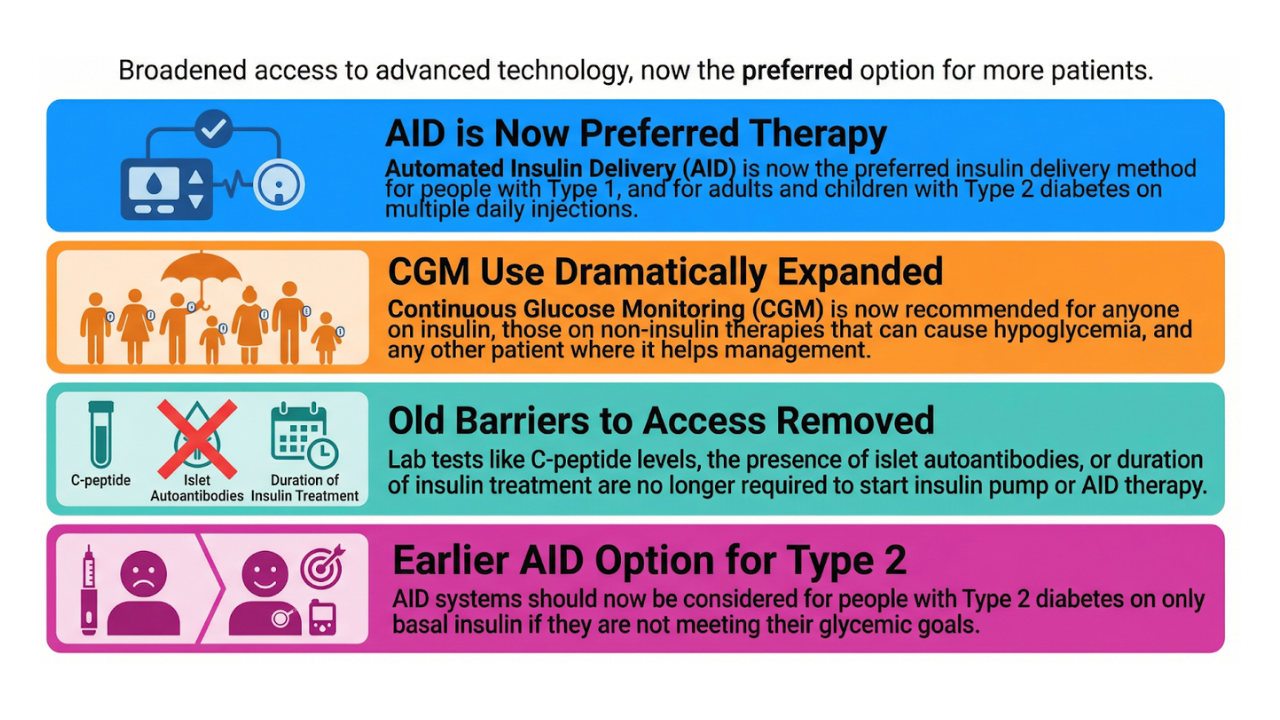
Abbott and Dexcom: different language, same destination
Despite different branding, Abbott and Dexcom are pursuing the same strategic shift.
Both are actively repositioning CGM from: a medical device for people with diabetes to a general-purpose metabolic insight tool for a broad population
Abbott: closing the behaviour loop
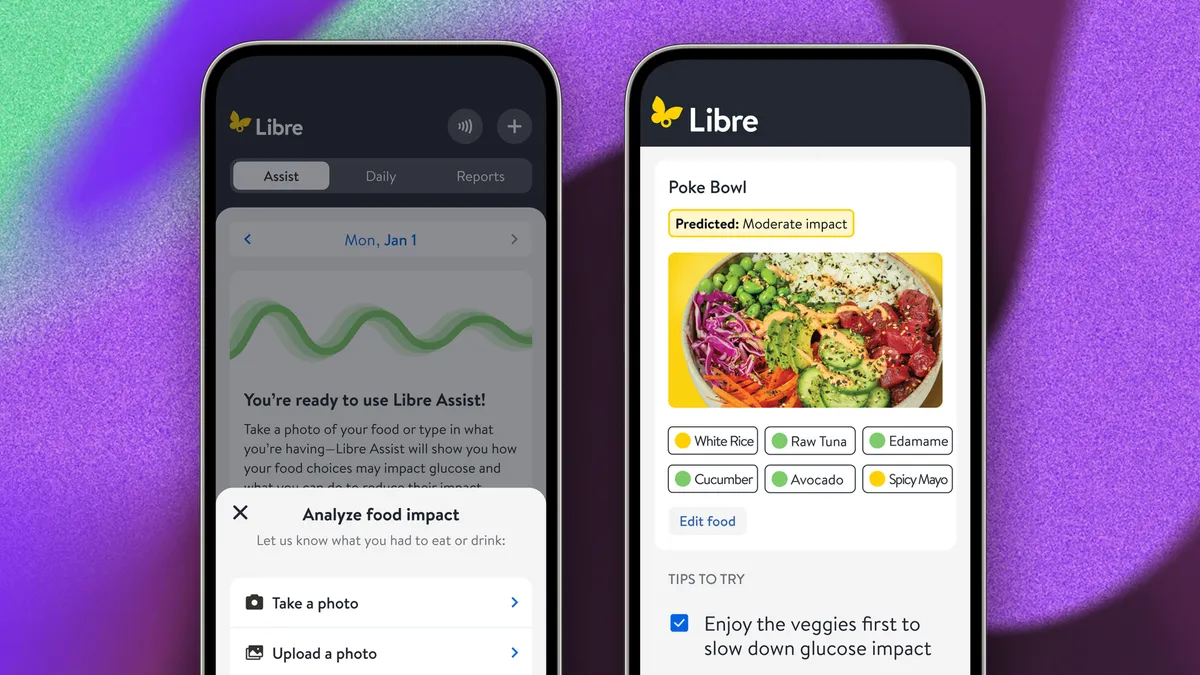
Image: An example of Libre Assist predicting how a poke bowl might impact your blood sugar.
Abbott framed glucose as an actionable signal.
With Libre Assist:
- Meals are photographed
- Glucose impact is predicted
- Users receive real-time suggestions to blunt spikes
The message is explicit: glucose is something you interact with, not something that happens to you.
Their messaging—reinforced by consumer ambassadors and partnerships like Weight Watchers & Withings—positions glucose as a daily optimisation signal inside lifestyle health.
Serena Williams took the stage to discuss her use of Lingo—not as a medical device, but as a learning tool. Her framing was simple and effective: “Health is number one.”
> Link to CES session with Serena Williams
Dexcom: normalising glucose as a health signal

Dexcom is expanding beyond diabetes into general health and wellness.
> Link to CES interview with Dexcom CEO Jake Leach
The reframing is deliberate:
- Not a disease marker
- Not a therapy trigger
- But a foundational physiological signal
Glucose is positioned alongside sleep, activity, and heart rate.
Stelo fits this strategy precisely: integration with Oura, smart food logging, and visualisation of glucose “load” from a photographed meal.
Different tone. Same direction.
CGM becomes consumer-owned, longevity-adjacent infrastructure.
What this means for healthcare professionals
This shift has real clinical consequences—whether we engage or not.
- CGM will often come before diagnosis
Patients will arrive with weeks or months of self-collected CGM data, outside reimbursement and without clinical framing.
The question shifts from “Should we start CGM?” to “How do we interpret the data they already have?” - Consultations move upstream
When patients already understand patterns and variability, our role shifts from education to interpretation: deciding which signals matter, which don’t, and what to act on. - More false certainty—and more clinical value
Consumer CGM and AI insights will sometimes mislead. That’s not failure; that’s where clinicians add value—by correcting, contextualising, and preventing overreaction. - Diabetes care becomes metabolic care
As glucose becomes a mainstream health metric, boundaries between diabetes, obesity, and cardiometabolic prevention continue to blur. This is not loss of expertise, but expansion of relevance.
Insulet: “Liveable Technology” enters CES

https://www.youtube.com/watch?v=-V11bVIlQAI
CES 2026 marked Insulet’s first appearance.
Omnipod 5 was framed not as pump therapy or AID, but as Liveable Technology—a lifestyle enabler for all insulin-treated people (type 1 and type 2).
Insulet reiterated that a fully closed-loop system for type 2 diabetes remains in development, with timelines pointing beyond 2028.
> Link to CES session from Insulet
Their framing echoed two broader societal trends:
- The "self-care healthcare" movement: people actively taking control of their health
- The "measure-me" movement: continuous tracking as a default behaviour
The implicit message to clinicians was clear:
Data availability is no longer the problem.
Meaning and guidance are.
The bigger signal: diabetes care is merging with everyday health
Across companies, the same pattern emerged:
- Less emphasis on disease labels
- More emphasis on continuous feedback loops
- Glucose positioned alongside sleep, activity, stress, and nutrition
This is not about replacing care teams.
It is about raising baseline health literacy before the consultation begins.
ChatGPT Health: the quiet structural shift

Away from the exhibit halls, one of the most consequential announcements last week came from OpenAI.
This formalises what is already happening: both patients and clinicians are using LLMs for health-related reasoning.
Health is already one of the most common use cases for ChatGPT.
OpenAI is now adding guardrails:
- a separate health data space,
- no training on health conversations,
- data isolation and encryption
- and user-controlled deletion.
At launch:
- Available in the US and Singapore
- Not available in the Europe, Switzerland, or the UK
- Web and iOS only (Android will follow later)
- Integration with Apple Health
- EMR connections via b.well and select US apps (MyFitnessPal, Weight Watchers, Peloton, Functions, AllTrails & Instacart)
This rollout lives or dies on trust.
The public reaction remains sceptical for now—particularly in Europe, where GDPR sets a higher bar.
Where ChatGPT Health is useful—and where it isn’t

Infographic > https://www.eesel.ai/blog/chatgpt-health
Clear value
- Preparing consultations
- Structuring questions
- Identifying cross-domain patterns
- Translating raw data into hypotheses
Clear limits
- Not diagnostic
- Not therapeutic
- No clinical liability
Two unavoidable concerns remain:
- Privacy: HIPAA-compliant is not GDPR-compliant
- Accuracy: LLMs can be confidently wrong
These tools augment cognition.
They do not replace judgment.
The consultation is changing—whether we like it or not

https://openai.com/index/introducing-chatgpt-health/?video=1152278055
The old model—uninformed patients, locked data, clinicians as sole interpreters—is eroding.
What replaces it can be better:
- More prepared patients
- More focused conversations
- Earlier pattern recognition
- Clearer cause–effect discussions
Our role evolves:
Not to compete with AI,
but to correct it, contextualise it, and challenge it.
Shorter consultations.
Deeper ones.
The real CES takeaway
CES 2026 did not announce a breakthrough diabetes tech device. It confirmed a trajectory.
Smarter patients. Smarter tools. Smarter clinicians — if we choose to engage.
AI will not replace physicians. But it will raise the intelligence floor of healthcare.
And that will likely change who walks into our consulting rooms — and how prepared they already are.
Kind regards,