The New ADA/EASD Type 1 Diabetes Adult Guidelines
Oct 22, 2025
At the EASD 2025 Annual Meeting in Vienna, Professors Anne Peters and Richard Holt presented the draft 2026 ADA/EASD Consensus Report on the Management of Type 1 Diabetes in Adults.
It updates the 2021 report—the most cited reference in adult type 1 diabetes management—to reflect new evidence in diagnosis, technology, cardiovascular risk, obesity, and psychosocial care.
In this post, we highlight the key updates from the 2026 draft, which was open for public comment until October 17. The final version will be published soon.
Yet beyond the data, one insight stood out: even in 2026, distinguishing between type 1 and type 2 diabetes remains surprisingly difficult.
After a century of progress, biology still resists simplicity.
“The more I learn, the more I realize how much I don’t know.” — Albert Einstein
Get Access To Updated Diabetes Technology Courses
1. Diagnosis: The Art of Uncertainty
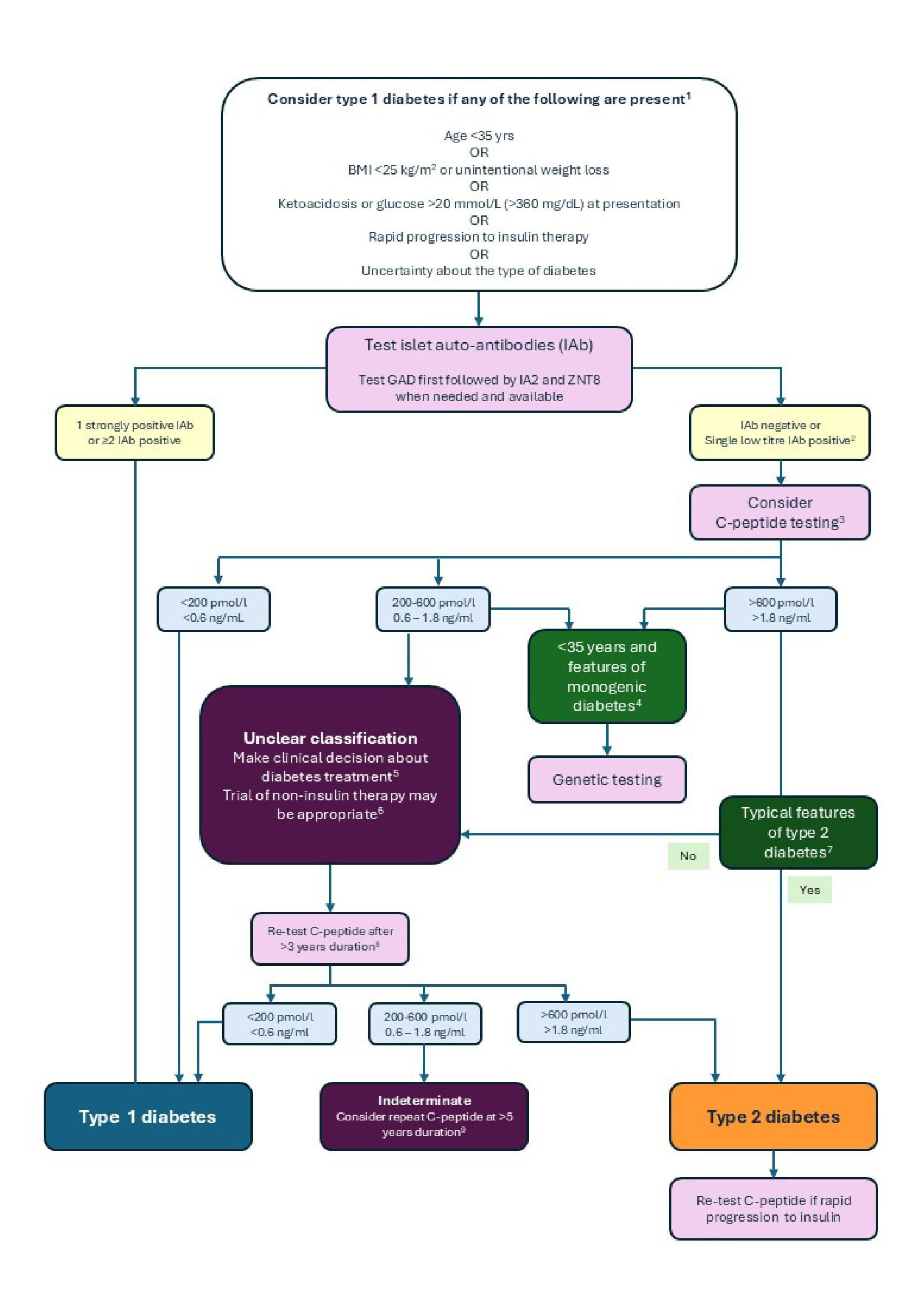
Figure > draft 2026 ADA/EASD Consensus Report on the Management of Type 1 Diabetes in Adults: Flowchart for investigation where type 1 diabetes is considered in adults
Adults rarely fit into neat categories.
The updated algorithm helps, but never eliminates ambiguity.
Clinicians are urged to suspect type 1 diabetes in adults < 35 years old, BMI < 25 kg/m², unintentional weight loss, diabetic ketoacidosis, or rapid progression to insulin within 3 years.
But many adults present with mixed features—autoimmunity and insulin resistance.
Autoantibody testing remains central:
- Measure GAD first; if negative, add IA-2 and ZnT8.
- A single low-titer autoantibody can be false positive.
- 5–10 % of adults with new-onset type 1 diabetes have no detectable antibodies, and antibody levels may fade over time.
C-peptide testing must now follow strict rules:
- Test within 5 hours of eating, and only interpret if the glucose is ≥ 72 mg/dL or 4 mmol/L.
- Avoid testing within 2 weeks of diabetic ketoacidosis (DKA) or 12 hours of hypoglycaemia.
- Be cautious in renal failure (C-peptide can appear falsely high).
C-peptide interpretation:
- < 200 pmol/L (< 0.6 ng/mL) → type 1 diabetes
- 200–600 pmol/L (0.6–1.8 ng/mL) → indeterminate zone
- 600 pmol/L (> 1.8 ng/mL) → type 2 diabetes
The report recognizes that LADA may be either a slower form of type 1 or an overlap condition
- and that some individuals can even have type 2 diabetes superimposed on type 1.
After every test, flowchart, and antibody panel, a small group still falls into the category “we don’t know.”
2. Glucose Management and Technology
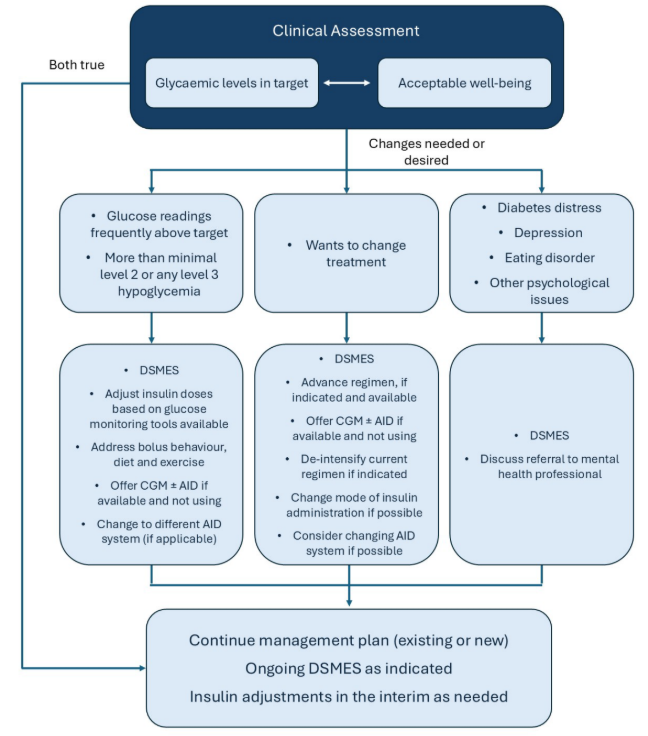
Figure > draft 2026 ADA/EASD Consensus Report on the Management of Type 1 Diabetes in Adults: A framework for the management of an individual with type 1 diabetes, considering both glycaemic levels and other psychosocial issues (DSMES: diabetes self-management education and support. CGM: continuous glucose monitoring. AID: automated insulin delivery)
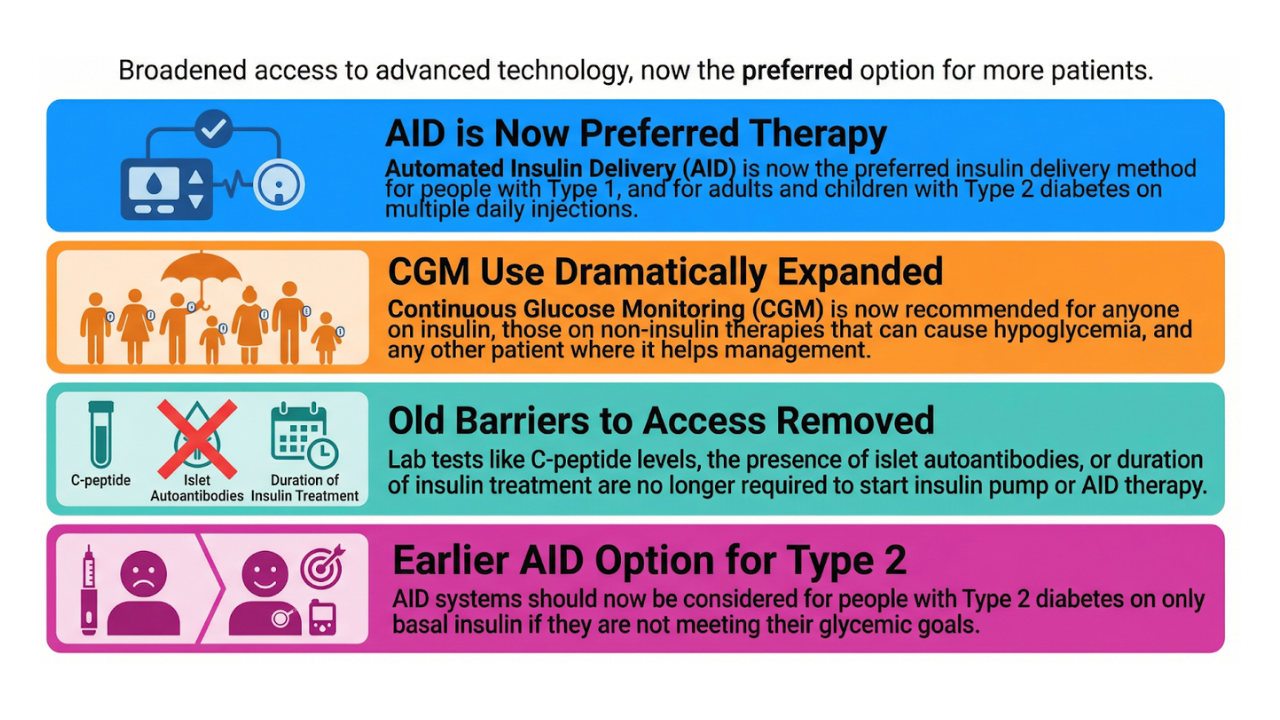
Continuous Glucose Monitoring (CGM) is reaffirmed as the standard of care for everyone with type 1 diabetes, with fingerstick testing as backup.
Automated Insulin Delivery (AID) systems are now the preferred insulin-delivery method, based on consistent data showing higher time in range (TIR), lower time below range (TBR), and a better quality of life.
For injection therapy, the recommendation remains:
- Multiple Daily Injections (MDI) using rapid-acting and long-acting analogues.
- Inhaled insulin (only available in the US and Brazil, soon also in India) is a safe alternative for meal boluses.
Importantly, the panel explicitly acknowledges open-source AID systems.
Clinicians should respect a person’s right to choose such systems and continue clinical support, even if unfamiliar with the specific algorithm settings.
CGM targets stay the same:
- TIR > 70 % (3.9–10.0 mmol/L)
- TBR < 4 % (< 3.9 mmol/L)
- Estimated HbA1c ≈ GMI < 7.0 % (53 mmol/mol)
3. Nutrition, Education, and Psychosocial Care
Nutrition therapy should be individualized.
- Low-carb or very-low-carb patterns can be safe if combined with balanced nutrition and close monitoring.
- The report warns that ketogenic diets can blunt glucagon responses and raise DKA risk, especially in insulin deficiency.
Carbohydrate counting remains the standard teaching method, though carbohydrate consistency can be an acceptable alternative.
DSMES (Diabetes Self-Management Education and Support) is emphasized as an ongoing process — at diagnosis, annually, and whenever life circumstances change.
Clinicians are encouraged to screen routinely for:
- Diabetes distress
- Depression and eating disorders
- Social determinants of health
Simple clinical questions still matter:
“Can you always feel when your blood sugar is low?”
“At what glucose level do you notice symptoms?”
They can identify impaired awareness of hypoglycaemia and prevent severe episodes more effectively than any app.
4. Adjunctive Therapies and Cardiometabolic Health
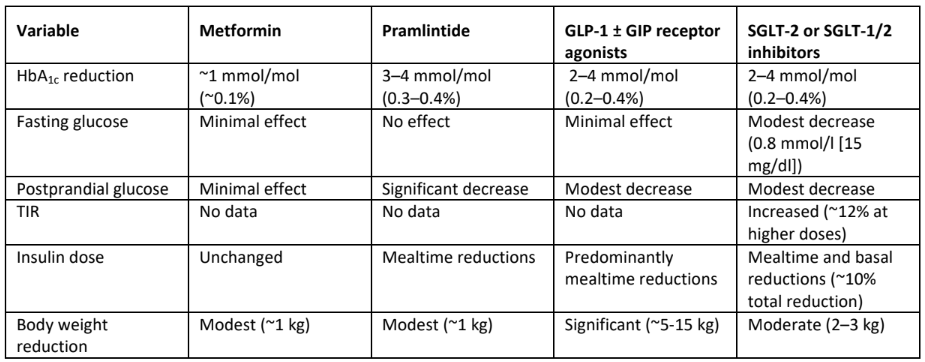
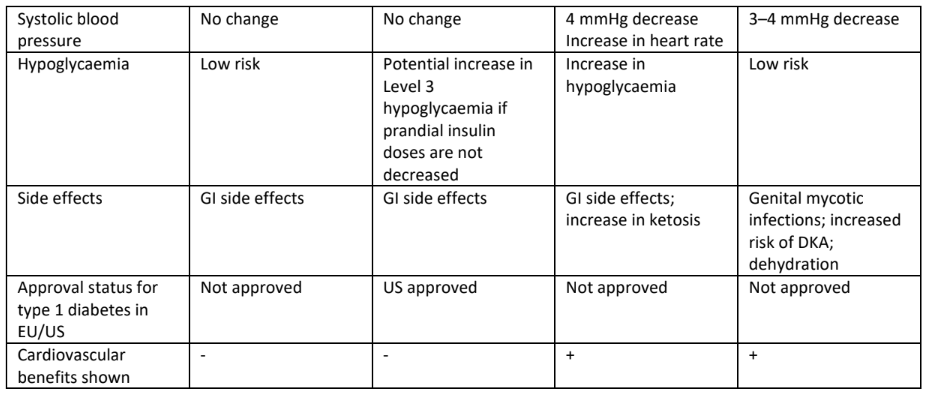
Table > draft 2026 ADA/EASD Consensus Report on the Management of Type 1 Diabetes in Adults: Adjunctive therapies for glycaemic management in type 1 diabetes.
For glucose control, evidence for using adjunctive therapies alongside insulin remains limited, and none are formally recommended.
But for cardiovascular protection, the tone shifts:
“A clear role for GLP-1 receptor agonists and SGLT2 inhibitors is emerging.”
The 2026 report also adds full sections on:
- Microvascular screening: same frequency and methods as type 2 diabetes, adjusted for risk.
- Cardiovascular prevention: treat blood pressure to < 120/80 mmHg; start statins in adults ≥ 40 years or younger if high risk.
- Obesity management: behavioral, pharmacologic (GLP-1 receptor agonists), and surgical options are valid in type 1 diabetes.
5. Special Populations
Older adults:
- Prioritize safety, simplicity, and hypoglycaemia avoidance.
- Continue CGM or AID if they support independence.
Hospital management:
- People who competently use CGM or pumps should, whenever possible, continue them.
- Target glucose 140–180 mg/dL (7.8–10.0 mmol/L); in non-critical cases, 100–180 mg/dL (5.6–10.0 mmol/L) is acceptable if achievable without hypoglycaemia.
Pregnancy:
- Addressed only briefly; clinicians are referred to ADA and EASD pregnancy guidelines.
6. The Takeaway
The new report doesn’t revolutionize diabetes care—it refines it.
It confirms the essentials: precise diagnosis, structured education, individualized targets, psychosocial screening, and equitable access to technology.
But it also exposes a deeper truth: even with every biomarker and algorithm, human metabolism resists simplicity.
Each discovery brings us closer to understanding, but also reveals how much remains unseen.
That’s why diabetes care demands not only science, but humility.
Ready to Go Deeper?
If you’d like to update your own knowledge on diabetes technology, you can now access a full library of independent e-learning modules created for healthcare professionals:
👉 Explore the courses at www.diabetotech.com
You’ll find concise, CME-accredited lessons on:
- Continuous Glucose Monitoring (CGM) — interpreting data, alarms, and TIR metrics
- Insulin Pump Therapy — practical setup, troubleshooting, and patient coaching
- Automated Insulin Delivery Systems (AID) — from commercial to open-source, including safety and clinical oversight
All courses are peer-reviewed, CME-accredited, and designed to translate technology into confident day-to-day practice.
Modules are available in English, Dutch, French, German, and Spanish.
Start here → www.diabetotech.com
Kind regards,