Do you want to know how C²GM works?
Jun 13, 2022
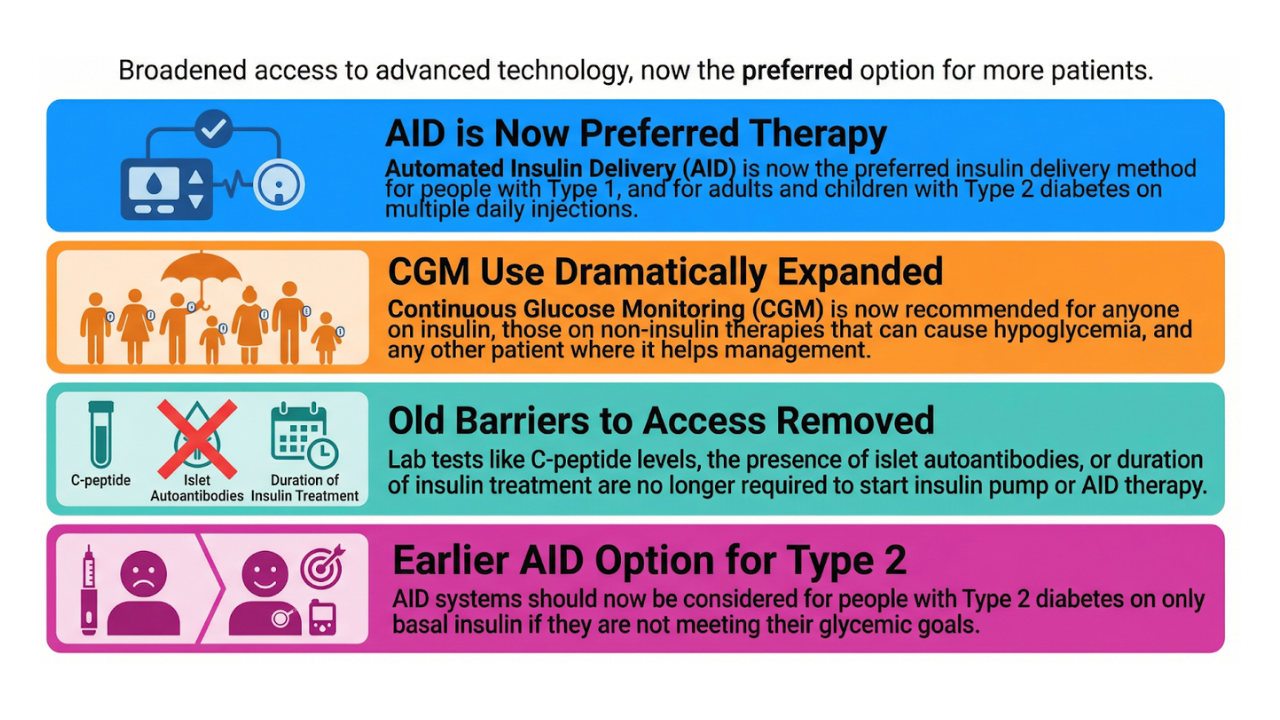
According to the ADA, anyone taking insulin should be offered continuous glucose monitoring (CGM). Although the reimboursement is not always there yet, many people are already doing this. We must prepare ourselves for this new CGM era, especially GPs who monitor a large proportion of people on insulin and will have to be able to give advice based on CGM data.
"Studies over the last year have made clear that if individuals are on insuline, no matter who or what age, they can benefit from CGM use." Dr. Robert Gabbay (Chief Science & Medical Officer American Diabetes Association)
How do you explain in an easy way how you can interpret and use the CGM data?
To this end, Dr. Bergenstal and Dr. Martens (International Diabetes Center Minnesota) have developed the C²GM model, and it was first shown at the ATTD and ADA this month. For the first set of guidelines, they focused on people with type 2 diabetes on basal insulin, usually followed up by their GP's.
In this article, I'd like to discuss these and other guidelines on how to interpret and use CGM data.
Get Access To Updated Diabetes Technology Courses
1. C²GM = CGM Clinician Guided Management
C²GM stands for CGM Clinician Guided Management and is a step-by-step plan for easily adapting the treatment of people with diabetes on the basis of CGM data. At the ATTD, Dr. Bergenstal presented the C²GM model for people with type 2 diabetes on basal insulin (basal-only), aimed at primary care (GPs). They first focused on this group because this is a very large group, and (according to them) they have the greatest need for a simple step-by-step plan. The majority of people with type 2 diabetes on 1 injection of basal insulin are not sufficiently regulated (69% of people on basal insulin have an HbA1c >7%). According to Dr. Bergenstal, this is not only due to therapeutic inertia, but also to the fact that our old way of (basal) insulin titration may not be good enough.
This is how we titrated basal insulin until now (according to Dr. Bergenstal):
- "treat to target" (set a target for fasting blood glucose, e.g. 110 mg/dl)
- "fix fasting first" (titrate basal insulin until target value is reached)
- and avoid "overbasalization", defined by a basal insulin dose >0.5 U/kg, a postprandial glycemia >180 mg/dl (or good fasting glycemia and an insufficiently controlled HbA1c) and/or a poor "BeAM score" (>Bed-AM: difference between the blood glucose at bedtime and the next morning > 50 mg/dl).
Now that we have CGM, however, we see a major problem of nighttime hypoglycemia in many people where we would normally (based on fingersticks alone) have tended to push basal insulin even further. It turns out that the lowest glycemia is not always in the morning, but sometimes also at night, something you can't see with finger pricks. This is one of the reasons why CGM is increasingly being promoted in everyone who uses insulin.
Many guidelines have been given in the past for interpreting CGM data. De Bergenstal once again repeated its 3-step analysis of an AGP profile (see also this blog post):
- More Green, Less Red: Look at the time-in-range (TIR) and time-below-range (TBR): is there a glucose problem?
- If so, where is the problem? Is the glycemic curve on the AGP profile Flat, Narrow & In Range?
- If not => titrate insulin
However, he now proposes to leave this roadmap for "CGM interpretation" and switch to a new "CGM action" plan, namely CGM Clinician Guided Management (C²GM). As mentioned, they first focused on people with type 2 diabetes on basal insulin (basal-only).
The following 3 step plan was developed:
- Determine if the patient has co-morbidities that require associating a GLP1 analogue or SGLT2 inhibitor (in accordance with ADA/EASD guidelines)
- Find the TIR and TBR and check if the TIR is >70% and the TBR is ≤2% (More Green, Less Red)
- Categorize patient and adjust therapy:
- TIR >70% and TBR ≤2: maintain current treatment, emphasize continued lifestyle changes and correct insulin intake. Schedule follow-up after 3-4 months.
- TIR >70% and TBR ≥2%: treat hypoglycemia by stopping sulphonylureas and/or reducing basal insulin if necessary. Schedule follow-up after 2 weeks.
- TIR <70% and TBR ≤2%: treat hyperglycemia by associating or elevating a GLP1 analogue, or raising basal insulin. Schedule follow-up after 2 weeks.
- TIR <70% and TBR ≥2%: treat hypoglycemia and refer to the diabetes educator/dietitian to address hyperglycemia by intensifying treatment (using a GLP1 analogue and/or mealtime insulin). Schedule follow-up after 2 weeks.
The latter is the most difficult group, with referral to an endocrinology team recommended. Below is the "cheat sheet" that their diabetes educators use to further titrate the (meal) insulin (if they had time):
With the C²GM model, you can divide your patient into 1 of the 4 treatment categories within a few seconds, based on the TIR and the TBR. It is remarkable that
- although the ADA guidelines recommend a TBR <4%, it was decided to start tapering the treatment from a TBR ≥2%. This is based on a revision of the Mobile Study AGP profiles (published last week in JAMA) by their own team. None of their team considered it safe to maintain or increase treatment as long as the TBR was not ≤2%.
- a follow-up after 2 weeks is suggested whenever treatment adjustment is made. In the past, it was recommended to see people every 3 months because an HbA1c check is only useful after 3 months. However, in the current CGM era, we can already see the effect of a therapy adjustment after 2 weeks. In the future, they would therefore like to create a new framework for diabetes care, moving away from the 3-monthly check-ups based on HbA1c.
- great emphasis is placed on the timely association of GLP1 analogues and SGLT2 inhibitors (in line with the ADA/EASD guideline). This is often difficult in Belgium due to limited reimbursement (eg GLP-1 analogues are only reimbursed if HbA1c >7.5% under Metformin and BMI >30, association with SGLT2 inhibitors is not reimbursed). Occasionally there are people who will pay for this themselves.
- people with type 2 diabetes who are older and at "increased risk" are not listed here. According to the ADA, the guidelines are a bit looser there, namely aiming for a TIR >50% and TBR <1% to guarantee safety. You should also keep that in mind.
In the future, they would like to test their C²GM model for people with type 2 diabetes on basal insulin in primary care, and integrate the CGM data into the EHR (electronic patient record). They have also developed a C²GM model for people with type 2 diabetes on basal-bolus insulin. This is already a lot more complex than the C²GM model for people on "basal-only" insulin, and is not intended for primary care, but for the diabetes team in 2nd line. (At a TIR <50% it is suggested here to try to redistribute the insulin to 50/50% basal/bolus insulin, and at a TIR 50-70% more specific trends are taken into account.)
All in all, I think this C²GM method is a very good way to easily adjust diabetes treatment based on CGM data. And although it is aimed at general practitioners, I also think it is a good way for endocrinologists and diabetes educators to work in a structured way. It is always useful to compare your own habits with the proposals of renowned endocrinologists that were discussed at both the ATTD and the ADA 2022. It is also useful for people with diabetes to know how you can properly adapt your treatment to the data from your CGM.
2. DATAA model
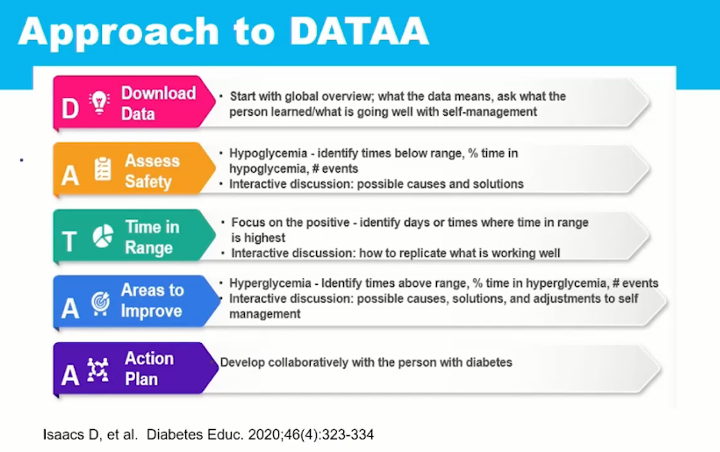
The C²GM method is of course not the first and last guideline for the interpretation of CGM data. For example, in 2020 the DATAA model was also published by Dr. Diana Isaacs.
This is a 5 step plan for a data-driven collaboration between the diabetes educator and the patient to improve self-care (cfr figure). As with the C²GM model, it is suggested to first evaluate safety and try to prevent hypoglycemia.
At the DATAA, however, there is more emphasis on focusing on what is going well, and encouraging behavior that gave a good TIR in the past.
3. Advanced CGM Education
Apart from the models for quickly interpreting CGM data, the ATTD also discussed guidelines for making better use of CGM data:
- "Alerts And Alarms Are Your Friends" Dr Edelman suggested at the ATTD to make more use of alarms. He systematically lowers the high alarm to <180 mg/dl in his patients to improve glycemic control. They don't do it with people with obvious alarm fatigue, but they do try to actively change the perception of alarms in everyone, namely that they can really help improve TIR. One way to combat alarm fatigue is, for example, to choose a more pleasant sound as the alarm (can only be done with Dexcom), and set the alarm only on certain parts of the day (can only be done with Dexcom & Guardian).
- Adjust the insulin dose according to the trend arrows. In that same session, the emphasis was placed on injecting more or less short-acting insulin based on the trend arrow. A handy trick is to add 50 mg/dl to the sensorglycemia shown with an upward arrow, and to add 75 mg/dl to a straight up arrow, then adjust the short-acting insulin based on of the schedule you are using. With an arrow down, they suggest waiting to give insulin until the arrow becomes flat again. Note: unlike the Libresensor, Dexcom and Guardian sensors also have a double arrow up and down (cfr diagram). These guidelines are also only valid for people who use insulin pens or a manual insulin pump (not for closed-loop systems).
- Finally, it was also suggested to print the AGP profile on the consultation and to have a discussion with the patient about achievable goals by next time. You can note the goals and the adjustments on the AGP profile and pass this on to the patient. Very often, what is said at the consultation is not remembered or is quickly forgotten, and that is a shame, of course.
Now it may all seem a bit complicated with CGM, but it really isn't! CGM provides much more data on glycemic control than fingersticks, and makes it much more intuitive. Just as patients don't want to go back to fingersticks once they've used CGM, it's hard for healthcare providers to start adjusting insulin based on fingersticks once you realize how much data you don't see compared to your previous patient with beautiful CGM-curves.
So don't be discouraged and let these models sink in. In any case, I will try to apply them by responding more quickly with a TBR >2% (in people with type 2 diabetes), seeing people again faster after a change in therapy, and also trying to give education about adjusting the insulin dose based on trend arrows.
And you? What will you change now that you have heard these guidelines?
Kind regards,