Advancements in Managing Type 1 Diabetes During Pregnancy: What's New?
Jun 12, 2023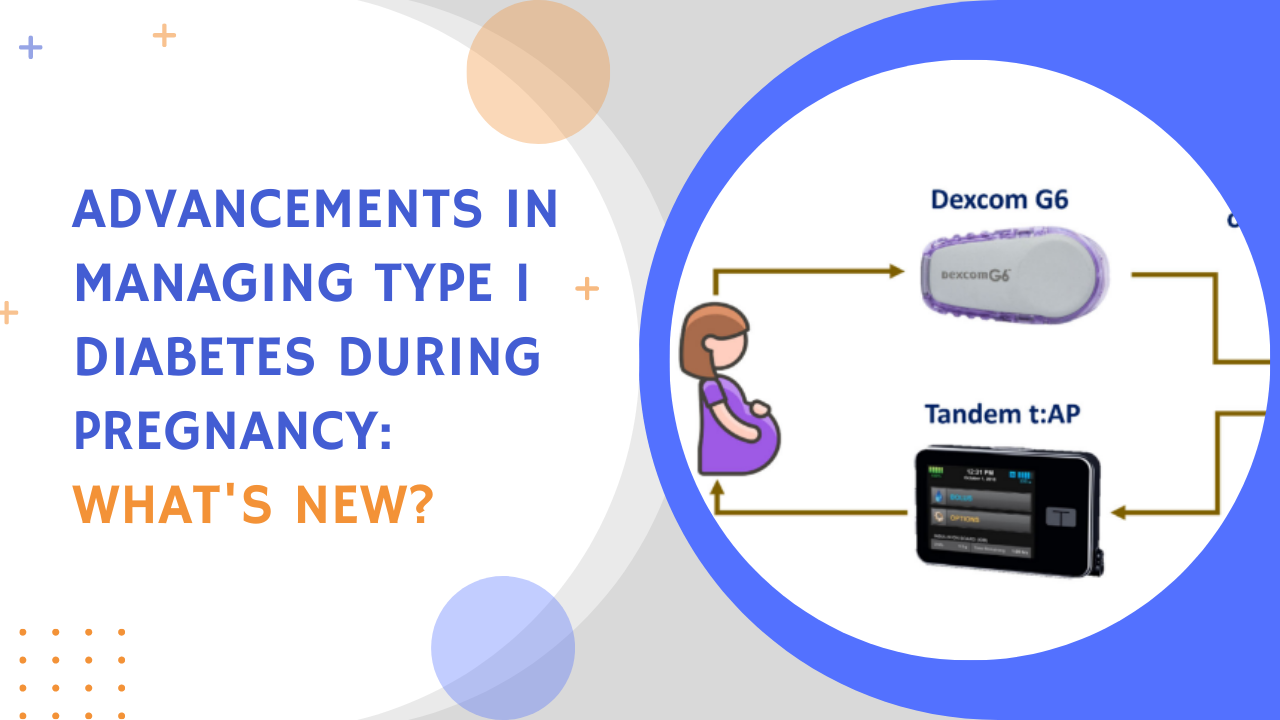
Pregnancy is a beautiful and transformative journey, but for women with type 1 diabetes, it requires extra attention and careful management of blood glucose levels.
The delicate balance of glycemic control becomes even more crucial during this time to ensure the health and well-being of both the mother and the developing fetus.
Fortunately, recent advancements in closed-loop systems have brought about significant progress in managing type 1 diabetes during pregnancy.
In this blog post, we will explore the latest developments in closed-loop systems and their potential to shape the future of care for pregnant women with type 1 diabetes.
Get Access To Updated Diabetes Technology Courses
Tailored Approaches to Glycemic Control
Achieving optimal glycemic control is of utmost importance during pregnancy. Healthcare providers have established specific guidelines to effectively manage blood glucose levels.
A recent publication (by dr Benhalima et al) gives a nice summary of the key recommendations:
- #1 Prepregnancy care: Women with type 1 diabetes should receive formal prepregnancy care to ensure they are in the best possible health before conception.
- #2 Adjusting insulin dose: Reducing insulin dose by 10-20% at 8-16 weeks gestation and limiting supplementary insulin between meals can help reduce the incidence of severe hypoglycemia in early pregnancy.
- #3 Screening for complications: Regular screening for complications like retinopathy and proteinuria should be conducted in each trimester to monitor progression and manage any issues promptly.
- #4 Safe insulin options: Insulin analogues like NovoRapid®, Humalog®, Fiasp®, Lyumjev®, Levemir®, Lantus®, Toujeo®, and Degludec® are considered safe for use during pregnancy. Results of a large randomized controlled trial with Fiasp in pregnant women with diabetes are expected in 2023.
- #5 Diabetic ketoacidosis (DKA): Pregnant women with type 1 diabetes should be educated about preventing, recognizing, and treating DKA, as they are at higher risk even at lower glucose levels (around 180-200 mg/dl or 10-11 mmol/l). DKA can have a high risk of fetal morbidity and loss (10-36%).
- #6 Carbohydrate intake: To prevent ketonemia, pregnant women with type 1 diabetes are advised to consume a minimum daily intake of 175 grams of carbohydrates. This amount of carbohydrate can be obtained by consuming 20 g at breakfast, 50 g at lunch, 50 g at dinner, and three snacks of 10–20 g during the day. A low-carbohydrate breakfast can prevent post-meal hyperglycemia caused by increased morning insulin resistance.
- #7 Timing of insulin administration: To accommodate for delayed absorption during pregnancy, inject short-acting insulin analogues 15 minutes before meals in early pregnancy, extending to 30-45 minutes before meals in late pregnancy.
- #8 Psychosocial support: Effective clinical and psychosocial support is essential for pregnant women with type 1 diabetes, as a lack of support and empathetic engagement from healthcare teams can negatively impact their psychological health and overall quality of life.
- #9 Peri/postpartum care: Continuation of intrapartum insulin pump therapy with CGM can be a safe option. After delivery, insulin doses should be reduced by at least 50% compared to late third trimester doses due to decreased insulin resistance. If breastfeeding, insulin requirements are approximately 20% lower than pre-pregnancy.
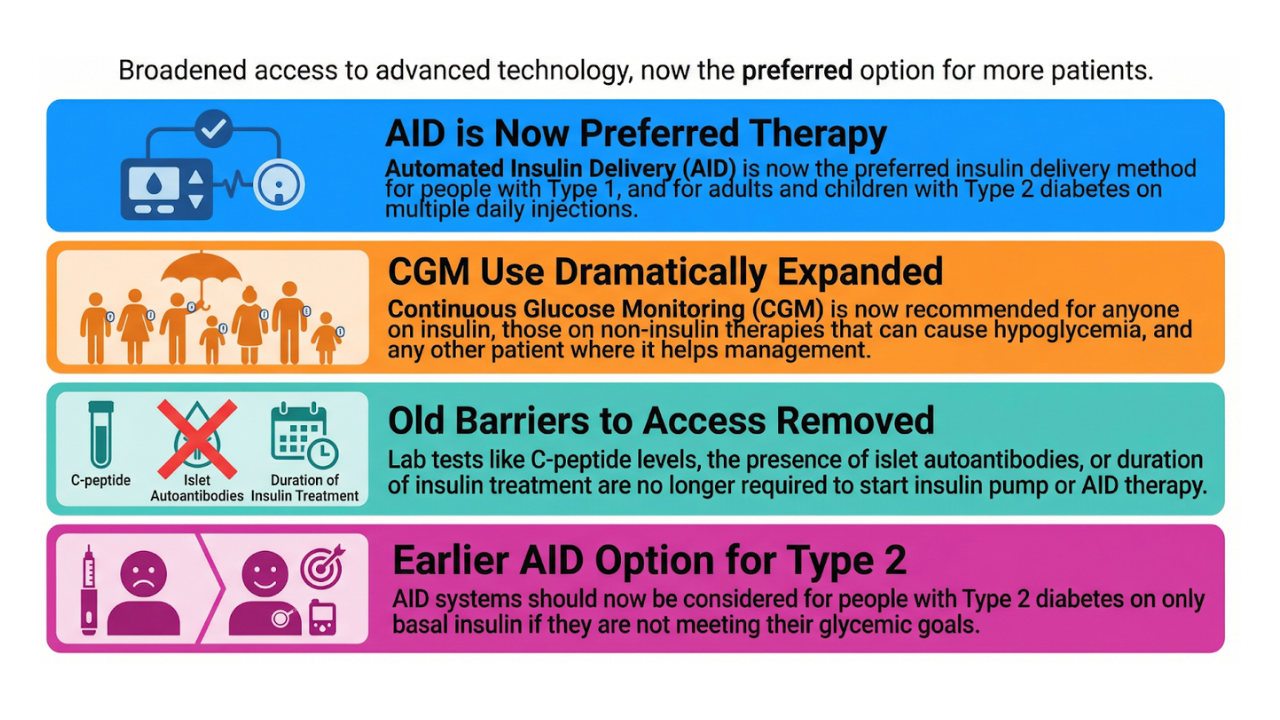
Adapted recommendations may be needed for Hybrid Closed-Loop (HCL) systems.
- Due to the automatic adaptation of the basal rate, bolus should be given 10–15 min before meals, but there might be less of a need to administer the bolus 30–45 min before meals in late pregnancy, as recommended when insulin pens or insulin pumps are used, although response should be individualised on the basis of each woman and system used.
- At ATTD online, dr. Benhalima shared that recent experience with the MiniMed 780G suggests that there is no need to adjust the SmartGuard target during and after delivery. Most women can maintain a target of 100 mg/dL (5.6 mmol/L) without experiencing hypoglycemia. However, individual adjustments may still be necessary based on specific needs.
- For more device-specific tips on how to use the different HCL in pregnancy, please check our previous blog.
The Potential of New Closed-Loop Systems: Pregnancy-Specific Zone Model Predictive Controller (iAPS)
Closed-loop systems with pregnancy-specific algorithms, such as the Pregnancy-Specific Zone Model Predictive Controller (iAPS), hold immense promise for optimizing glycemic control during pregnancy.

The iAPS is a novel, user‐friendly, smartphone‐based artificial pancreas platform that integrates Dexcom G6 CGM and Tandem t:AP research insulin pump.
- The iAPS app has an intuitive user interface, allowing participants to request insulin boluses, log activities, and receive alerts for various events.
- The system targets a range of 80-110 mg/dL (4.4-6.1 mmol/l) during the day and 80-100 mg/dl (4.4-5.6 mmol/l) during the night (12:00 AM-6:00 AM).
- Meal boluses are automatically reduced by 20% if premeal glucose is below 70 mg/dl (3.9 mmol/l).
- Correction boluses are administered to bring glucose to 90 mg/dl (5 mmol/l) if the premeal glucose is above 100 mg/dl (5.6 mmol/l).
- The controller intensifies basal insulin delivery when the blood glucose values trend upward while in the 120–180 mg/dl (6.7–10 mmol/l) range.
- The system includes a health monitoring system, which provides audiovisual advisory alarms and sends text messages to the research team for impending hypoglycemia.
A recent publication in Diabetes Care demonstrated the efficacy and safety of iAPS in 10 pregnant women with type 1 diabetes, showing
- increased pregnancy-specific time in range (TIRp) from 65% to 79%
- and a decreased time below range (TBR) from 3.7% to 1.6% during the trial period.
These study results confirm the feasibility of pregnancy-specific closed-loop control, demonstrating effective glycemic control without severe adverse events or increased hypoglycemia.
Larger studies and participant satisfaction surveys are needed to explore generalizability further.
Collaborative Networks and Future Research
At the moment we are waiting on the results of 4 big RCT's about different closed-loop systems in pregnancy:
- PICLS - 24 pregnant women with type 1 diabetes on MiniMed 670G - completed in March 2022, results expected at ADA2023
- AiDAPT - 62 pregnant women with type 1 diabetes on CamAPS FX - completed in Nov 2022, results expected at ADA2023
- CRISTAL - 46 pregnant women with type 1 diabeten on MiniMed 780G - completed in April 2023, results expected in 2024
- CIRCUIT - 33 pregnant women with type 1 diabetes on Tandem Control IQ - expected completion in jan 2024
Untill now, all studies have primarely aimed at assessing glycemic outcomes.
To further understand the impact of closed-loop systems on pregnancy and neonatal outcomes, large-scale collaborative studies are necessary.
Notably, the AiDAPT, CRISTAL, CIRCUIT, LOIS-P, and PICLS investigators aim to conduct a meta-analysis in the future.
- By pooling data from various studies, they can increase statistical power and analyze pregnancy outcomes and patient-reported outcomes comprehensively.
- In addition, this meta-analysis will also include participant-reported outcomes to identify the psychosocial effect of hybrid closed-loop use in pregnancy.
These collaborative efforts will provide valuable insights into the benefits of closed-loop systems and pregnancy-specific algorithms in managing type 1 diabetes during pregnancy.
Conclusion
The management of type 1 diabetes during pregnancy poses unique challenges, but advancements in closed-loop systems offer new hope for improved outcomes.
Tailored approaches to glycemic control, along with pregnancy-specific algorithms like iAPS, will provide personalized and precise management options in the future.
Ongoing research and collaborative networks are expanding our understanding of the benefits of closed-loop systems, not only in terms of Time in Range (TIR) but also in improving pregnancy and neonatal outcomes.
To make choosing a closed-loop system easier for people with type 1 diabetes, we have developed a 10 best closed-loop systems cheat sheet.
Get the cheat sheet here, so you can select the closed-loop system that would be a good fit for you or your patient!
Let's spread the word and keep up our efforts towards improving treatment options for moms with type 1 diabetes!
Kind regards,