Skin Issues Caused by Diabetes Devices: Tips for Prevention and Treatment
Nov 07, 2023
Skin problems are a common side effect for people using sensors and insulin pumps. At the ISPAD (International Society for Paediatric and Adolescent Diabetes) Congress 2023, the first results were shared from the SKIN-PEDIC study, which sought to identify these problems. The findings highlight the importance of awareness and proactive care to prevent and treat skin reactions.
Get Access To Updated Diabetes Technology Courses
In this blog post, we will go over the results of the SKIN PEDIC study,
along with the tips given to prevent and treat these skin problems.
"It's really important when you use diabetes devices, that you are aware that you can get skin reactions, and that many actually do have certain skin problems. We as healthcare professionals need to be aware of it, and look at the skin, and also try to help them in order to intervene in the early phases of the reactions. You can prevent some of the reactions by good skin care, mainly the wounds and the skin injury. For the eczema reaction you need to often use patches underneath." - Dr Anna Korsgaard, endocrinologist Steno Diabetes Center, Denmark, ISPAD2023
1. SKIN-PEDIC study
The SKIN-PEDIC study was conducted in 20 diabetes centres worldwide, where children and adolescents under the age of 18 were surveyed about their experiences with diabetes devices.
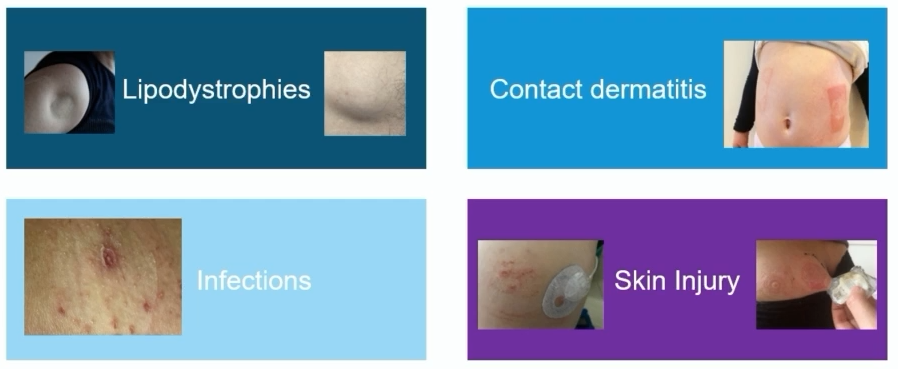
The skin problems were divided into four categories, namely:
- skin lesions (wounds and scars)
- eczema (contact dermatitis)
- infection
- lipodystrophy (lipohypertrophy or lipoatrophy)
The results were presented by Dr Korsgaard (Steno Diabetes Center, Denmark) at ISPAD2023, a publication will follow:
|
Pump users (n=1146) |
Sensor users (n=1166) |
|
|
Old scars |
33% |
17% |
|
Eczema (contact dermatitis) |
8% |
9% |
|
Wounds |
6% |
3% |
|
Infection |
2% |
1% |
|
Lipohypertrophy |
12% |
1% |
|
Lipoatrophy |
3% |
0% |
Besides these 4 categories of skin problems, the most common complaint of people is itching.
- This occurs in 23% to 77% of people who wear an insulin pump or sensor.
- Itching can lead to reduced concentration at school, sleep problems, and the device loosening from scratching.
- Scratching also deteriorates the skin barrier, and you are back more likely to have skin problems.
As a healthcare provider, it is therefore important to be aware of, and actively question, the high prevalence of skin problems with sensor and pump use.
Problems usually occur 4-10 months after starting the device, and the main symptoms are itching, pain and redness.
Moreover, it is essential to check the skin for lipodystrophy, as this still occurs in more than 10% of pump users.
By responding in time, bigger problems can be avoided.
2. "Skin Care Programme" to prevent skin problems
Dr Korsgaard also discussed their Skin Care Program, which can be downloaded for free at this link.
In it, you will find the following tips to avoid problems:
- Good skin care:
- Use unperfumed skin products and soap
- Use daily lipid lotion on the so-called "pause sites", these are the infusion sites where you are currently not wearing a device (in this Danish skin programme, reference is made to Decubal Lipid Lotion 70%, however in the pharmacy you can also ask for a similar cream)
- Careful application and removal of the device
- Avoid alcohol wipes, but clean the skin with soap and water
- Firstly loosen the sides of the patch before slowly removing the device at a low angle ("low and slow")
- Use a solvent to remove glue residue (you can also ask for this at the pharmacy)
- Consider an overpatch in case of loosening of the device
- Consider alternative barriers in case of irritated or dry skin:
- Liquid barrier that must dry before device placement (e.g. barrier cream or barrier spray)
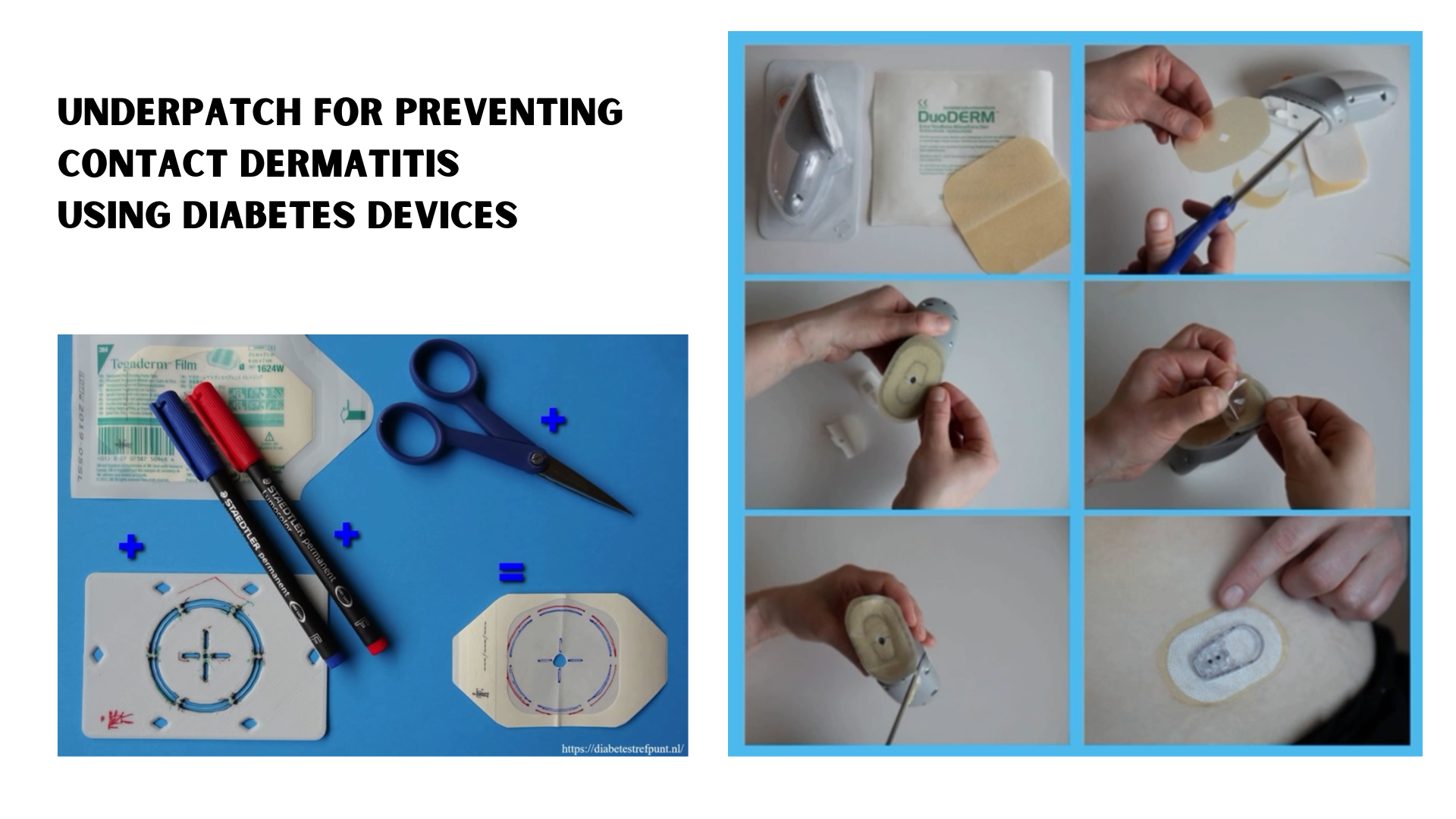
- Thin underpatch (e.g. IV3000, Leukomed, Fixomull or Tegaderm)
- Thicker underpatch (e.g. Duoderm or Compeed)
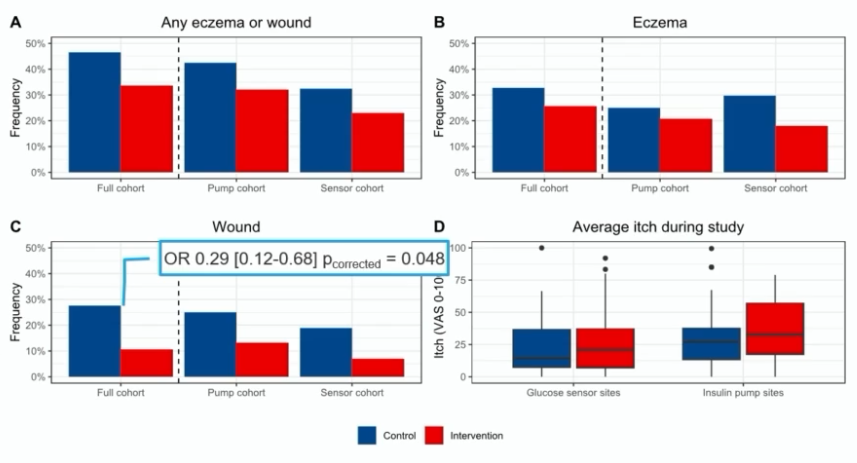
With this Skin Care Program, Dr Korsgaard was able to show that the incidence of skin problems in children and adolescents reduced from 47% to 34% after 1 year (Korsgaard et al. Diabetes Care 2023).
- In particular, the number of wounds could be significantly reduced.
- For eczema and itching, there was little effect, and further research is needed.
3. Tips to treat skin problems
Once there are skin problems, some treatment tips were also given:
- Let the skin problem heal by choosing another insertion site.
- If necessary, use cortisone ointment temporarily. Choose a preparation with weak corticoid action and limit use to 4 weeks to prevent secondary skin atrophy.
To prevent new skin problems, you can try the following:
- Use a barrier cream or spray.
- Use an underpatch. Above you can see some examples of how the underpatches can be cut to fit the Libre and Dexcom sensor.
- You can also use cortisone nasal spray at the insertion site before placement. However, it was noted that the local use of cortisone spray under a device has not yet been studied for safety, and theoretically, it cannot be ruled out that it could lead to skin atrophy in the long term.
The SKIN PEDIC study also asked about the methods used to treat skin problems:
|
Pump users (n=1146) |
Sensor users (n=1166) |
|
|
Barrier spray/cream |
11.9% |
10.0% |
|
Overpatch |
5.6% |
6.4% |
|
Underpatch |
2.2% |
2.6% |
|
Cortisone nasal spray |
1.4% |
1.4% |
Although underpatches are suggested here as a good solution to experience less irritation, they are currently relatively little used.
Regarding lipohypertrophy, the importance of education about reduced insulin uptake at that site was highlighted, even though it is often less painful to place the infusion set in that area.
- If you want more information on recent research on lipohypertrophy, you can also visit the Diabetes Technology Society's free webinar.
- Some people also use echography to identify lipodystrophy or to indicate suitable infusion sites with sufficient subcutaneous adipose tissue.
- Occasionally, localised hyperechogenicity is also observed at the infusion site (Sorensen et al, DTT 2023), but the significance of this is not yet fully understood.
Regarding lipoatrophy, there is research suggesting that it may be more interesting to switch to another insulin variant (Kordonouri et al, Pediatric Diabetes 2020).
4. Recognise high-risk individuals
Dr Thomas Rustemeyer, a dermatologist from Rotterdam, showed at ISPAD2023 how to spot people at increased risk of skin problems.
- Children already have naturally more sensitive skin.
- People with a past history of contact dermatitis are also more susceptible to recurrence of this condition.
- And people with atopic dermatitis are as much 30 times more likely to have skin problems when using diabetes devices.
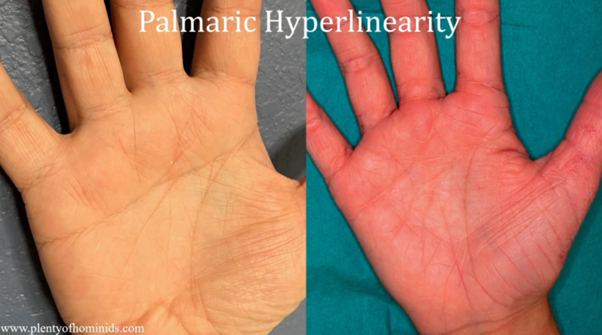
People with atopic dermatitis can apparently be identified very easily:
- You can ask if they tolerate wool on bare skin (if it feels uncomfortable, this may indicate atopic dermatitis)
- Or you can look at their palms (many small lines on the palms are characteristic of atopic dermatitis)
5. Exclude contact allergy

Distinguishing between contact irritation and contact allergy can be difficult.
Dr Rustemeyer therefore recommended that when an eczematous reaction occurs, allergy tests should be performed and, if possible, the allergen should be avoided.
Major allergens include
- the adhesives of the devices (epoxy resins, methyl acrylate, colophony),
- preservatives,
- antioxidants,
- silicone
- and metals.
New adhesives are constantly being developed, so new allergens are also constantly being discovered.
There was therefore a clear call for manufacturers to provide more clarity on the products used in their devices,
to better understand what triggers these reactions.
As more people turn to sensors and pumps, the likelihood of skin problems arising increases.
Dr. Korsgaard concluded on a positive note, stating that "every person with diabetes should be able to use diabetes devices without encountering skin problems."
We found great encouragement in the significant ongoing research in this field, showing the active commitment of many individuals to address these concerns.
If you're seeking comprehensive information on sensors and pumps and essential guidelines for their proper use, we have just launched free YouTube courses last week.
▶️ Click this link to explore and learn more. ◀️
Don't let skin problems hinder your diabetes care.
Kind regards,
Inge