HbA1c: a thing of the past?
Dec 13, 2021

According to Dr. Bergenstal, we are slowly moving from the "HbA1c era" to the "CGM+ era".
At the Virtual Diabetes Technology conference last month, he explained that we need to bridge to 2 eras by making CGM data more interpretable. We saw an update to the well-known "AGP report" and an example of a combined CGM parameter, that could serve as a replacement for HbA1c.
In this blog I describe:
- what the "Beyond A1c" movement is
- why CGM data may predict diabetes complications better than HbA1c
- why there is a difference between estimated HbA1c (>CGM data) and measured HbA1c
- what the latest update of the AGP report looks like
- and how combined CGM parameters like the "Glycemia Risk Index" can help.
Although HbA1c is not currently being abandoned (if only because we can't expect everyone with diabetes to have CGM any time soon), it is clear that CGM is becoming the standard of care for glycemic control in people with diabetes, especially those taking insulin.
Get Access To Updated Diabetes Technology Courses

1️⃣ "Beyond A1c" movement
The ADA and diaTribe have long argued for using CGM data, such as Time In Range (TIR), Time Below Range (TBR) and Glycemic Variation (GV), in addition to HbA1c because:
- HbA1c says nothing about diurnal fluctuations in glycemia (even with good HbA1c there can be significant hyper/hypoglycemia or glycemic variability)
- HbA1c says nothing about how we can improve glycemic control
- HbA1c can only be monitored every 3 months
- HbA1c may be falsely high or low (as with abnormal RBC turnover, transfusions, hemoglobinopathies, or certain races)
- and there are more and more people who have CGM available (although in my opinion there are still too few).
Especially in times of corona, CGM data have proved useful because more people were monitored virtually, and not everyone had their HbA1c checked regularly. In addition, the HbA1c can also be estimated from the CGM data, so that the same value can continue to be used in the follow-up.
HbA1c therefore does not have much added value for people who use CGM. For now, HbA1c is not completely abandoned, as it remains the best-studied predictor of diabetes complications, providing a better picture of glycemic control over the past 3 months.
On the other hand, we now know that CGM data are also related to diabetes complications, and theoretically you can also draw the CGM data from the past 3 months (although in practice this does not happen due to time constraints).
2️⃣ CGM data may be more correlated with diabetes complications than HbA1c
In recent years, one study after another has shown that TIR, the most important CGM parameter, is strongly correlated with diabetes complications:
- TIR ~ retinopathy and microalbuminuria in DM1 (Beck et al. Diabetes Care 2018)
- TIR ~ retinopathy in DM2 (Lu et al. Diabetes Care 2018)
- TIR ~ peripheral neuropathy in DM2 (Mayeda et al. BMJ Open 2019)
- TIR ~ carotid intima media thickness at DM2 (Lu et al. DTT 2020)
- TIR ~ albuminuria in DM1 (Ranjan et al. Diabetes Care 2020)
- TIR ~ albuminuria in DM2 (Yoo et al. DTT 2020)
- TIR ~ MACE in DM2 (Bergenstal et al. Diabetes 2020)
- TIR ~ cardiac autonomic neuropathy in DM2 (Kim et al. DTT 2021)
- TIR ~ mortality in DM2 (Lu et al Diabetes Care 2021)
Most key opinion leaders at the Virtual Diabetes Technology Meeting indicated that there is enough data for them to believe that TIR can be used to predict diabetes complications. It was therefore again asked to include CGM data when evaluating diabetes medication.
A recent article in the Lancet explains that HbA1c is not the best parameter for diabetes complications anyway. For example, a study in Sweden showed that people with type 1 diabetes with an HbA1c <7% had 2 times the risk of dying than people without diabetes. This may be because HbA1c does not sufficiently take into account other aspects of glycemic control, such as glycemic variability, TIR, TBR and acute hyperglycemia (postprandial and after hypoglycemia). For all these parameters a direct correlation with diabetes complications has already been demonstrated.
Of course, we don't have 40 years of data as with HbA1c, and the relative importance of all these parameters is not yet clear. But it may well be that in the future CGM data will be more relevant than HbA1c in predicting diabetes complications.
3️⃣ Relationship between HbA1c, estimated HbA1c and TIR
We know that the HbA1c correlates well with the TIR, but the corresponding values vary from study to study. In general you can say that 10% TIR corresponds to 0.5% HbA1c.
CGM data of 10-14 days can provide a good estimate of the past 3 months, and HbA1c can be estimated if 70% of the measurements are available. This estimated HbA1c (eHbA1c) is called the GMI (= Glucose Management Indicator), and is calculated from the mean glycemia from CGM data: GMI (%) = 3.31 + 0.02392 x (mean glycemia in mg/dl). An average glycemia of 150 mg/dl corresponds to a GMI of 7% with this formula.
In practice, however, there are often relevant differences between the GMI and the HbA1c:
- The GMI is typically lower than the HbA1c, especially if the HbA1c is >8% or the GMI >7.5%, but not all studies show the same (cfr study in Flanders and Wallonia).
- The difference between GMI and HbA1c usually remains the same in the same patient (although this study in Flanders was unable to demonstrate this).
The difference between GMI and HbA1c is probably due to the difference in the rate of glycosylation of the blood, and the lifespan of the red blood cells. While the HbA1c gives "false low" or false high" results in pregnancy, renal insufficiency, iron deficiency, anemia and the like due to varying red blood cell turnover, the GMI will not depend on this. To address this, a proposal was recently published to switch to “adjusted HbA1c”, which also takes into account the longevity of red blood cells.
The question, of course, remains which mean glycemia is most relevant: that in the blood (HbA1c) or that in the interstitium (GMI)? In any case, both are clearly related to diabetes complications. Importantly, both HbA1c and GMI are only estimates of glycemic control, and neither provide a complete picture of glycemic control.

4️⃣ Evolution of the AGP report
To make the interpretation of CGM data easier, CGM firms are asked to display the data in an AGP report.
The targets were set in an international consensus in 2019, and added to the AGP report. Some highlights are:
- TIR must be >70%. An improvement of the TIR of 5% is a clinically relevant result (cfr. this corresponds to a HbA1c decrease of 0.3%).
- TBR should be <4%. It is better to discuss the number of minutes rather than the number of % <4%, as this will be more clear to the person with diabetes (1% = 15 minutes).
- the glycemic variation (GV) should be <36%. This will of course be easier to achieve in people with type 2 diabetes than in people with type 1 diabetes. If GV is >36%, we speak of an unstable glycemia, and there is a significantly higher risk of hypoglycemia.
Dr Bergenstal explains in the following video how you can interpret an AGP profile the fastest:
- First, look at the top 10 core parameters panel of the AGP report to see if there is a problem.
- If yes, look at the AGP figure to see where the problem is, and treat hypos first. The aim is to get "More Green and Less Red" (MGLR) and to get the curve as "Flat, Narrow and In Range" as possible (FNIR)
- Before making any adjustments, look at the bottom panel of the AGP report with the daily patterns, to make sure that the pattern is not only on work or rest days.
Abbott, Dexcom, Sensionics and Diasend/Glooko offer their CGM reports in the AGP format in their reading software (not yet on their mobile apps). Medtronic and Tandem are not participating for the time being, which is a shame. Tidepool also currently has insufficient funding to purchase and implement an AGP license (such a license would cost USD 10-50,000). Roche, Ascencia, Lifescan, DreaMed and Bigfoot have the license, but I haven't seen an implementation of this yet.
A new update of the AGP profile was presented at the Virtual Diabetes Technology Meeting last month. The most important changes are a more streamlined top panel (less text), and a coloring of the AGP profile, so that the hypos stand out more. Especially now that more and more blood glucose meters are also incorporating the TIR concept in their reports (Lifescan, Dario and Roche), it is important that the TIR colors are standardized and not used interchangeably (as is now the case).

5️⃣ Glycemia Risk Index
To get a complete picture of the glycemic control, you should not only look at the HbA1c or the TIR, but also at the TBR and the glycemic variation, among other things. In order to gain insight into complete glycemic control in a faster way, people have been looking for 1 combined parameter for glycemic control (such as the HbA1c of the past). Several proposals have already been made in the past:
- Average Risk Range in 2006,
- GRADE in 2007,
- Blood Glucose Risk Index in 2009,
- IGC in 2009,
- Hypoglycemia-A1c score in 2015,
- Q-score in 2015,
- Personal Glycemic State in 2017,
- Compehensive Glucose Pentagon in 2017,
- Hypo-Triad in 2018,
- COGI in 2019,
- Glycemische Heptagon in 2021,
- Glycemic Deviation Index in 2021.
At the Virtual Diabetes Technology Meeting, Dr. Klonoff (the president of the Diabetes Technology Society) presented the Glycemia Risk Index or the Dysglycemia Index (the name is still in doubt). This parameter (0-100) scores 7 CGM parameters according to their relevance (based on the opinion of 330 physicians and 80 researchers), and divides the results into 5 percentiles or "glycemia zones". The higher the result, the worse. Further research will investigate whether this parameter is really related to diabetes complications.
In the subsequent presentation, dr. Bergenstal proposed a holistic AGP profile that, in addition to the new "Glycemia Risk Index", also includes the presence of cardiovascular risk, heart failure and renal insufficiency, and a diabetes distress score.
Like many other centers, the Diabetes Center Bern and DD Analytics are also planning further research into new glycemic control scoring systems. The future will show how the AGP report will evolve, which parameters will still be added, and what the best trade-off is between interesting data and "information overload".
In any case, it is clear that CGM parameters and therefore also CGM use is important to adequately control glycemia and avoid diabetes complications, in both people with type 1 and type 2 diabetes.
We have recently seen a lot of movement in other countries:
- Ontario (Canada) is leading by example and has reimboursed FGM/CGM for everyone with diabetes on insulin since 11/30/2021.
- Although there is already a broad reimbursement for FGM in the Netherlands, they continue to fight for more reimbursement for CGM.
- The National Institute for health and Care Excellence (NICE) in England recently published guidelines recommending wider use of FGM/CGM.
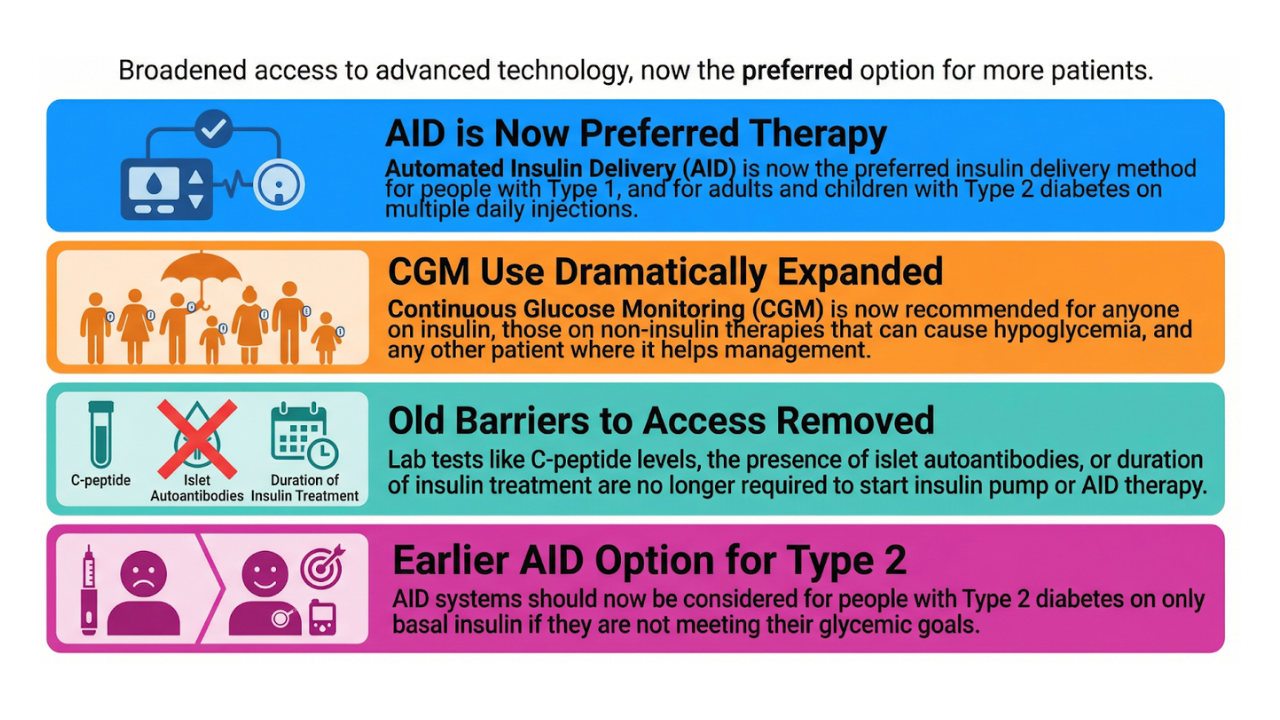
- In America, the eligibility criteria for CGM were recently broadened. The ADA, meanwhile, is also trying to get Medicare reimbursement for CGM in people who inject less than 3x/d insulin.
In Belgium, CGM is only reimbursed for people with type 1 diabetes or in the group A diabetes convention. This means that someone with type 2 diabetes who uses insulin 4x/d still has to prick their finger 4x/d... Of course we hope that this will soon be adapted to the current standard of care!
Kind regards,