December update (EN)
Jan 05, 2023
It's Christmas break and the temperatures may be dropping, but there is never a shortage of news and updates in the field of diabetes technology!
If you are a caregiver or live with diabetes, and want to stay up to date on the latest news about diabetes technology, check out this December update.
In this blog post, we take a look at what has changed in the world of diabetes technology over the last month, so you can make sure you have everything up to date before you head into the new year.
Get Access To Updated Diabetes Technology Courses
- Dexcom G7 approved by the FDA (8-12-2022)
- Publication ADA Standards of Care 2023 (22-12-2022)
- Publication international consensus around use of CGM in clinical trials (6-12-2022)
- Tandem bought Swiss Sigi insulin pump (13-12-2022)
- Lilly will not distribute YpsoPump in US (9-12-2022)
Read on below!
1. Dexcom G7 was approved by the FDA on 8-12-2022

What are the differences between Dexcom G7 and Dexcom G6?
Dexcom G7 is the successor of the Dexcom G6.
The main differences from the Dexcom G6 are:
- that Dexcom G7 is 60% smaller,
- it's a sensor and transmitter in one,
- it has a warm-up time of 30 minutes instead of 2 hours,
- that it lasts 10.5 days instead of 10 days ("12-hour grace period"),
- and that the accuracy would be slightly better (MARD 8.2% instead of 9% with Dexcom G6).

Minor differences between the Dexcom G7 and the Dexcom G6 are that:
- you can more easily see your time-in-range in the Dexcom G7 app (the Dexcom Clarity app was integrated),
- the applicator and receiver for the Dexcom G7 are smaller,
- the Dexcom G7 can connect to 3 devices at the same time, making a direct-to-(Apple)watch feature possible in the future,
- the urgent low alarm can be silnced and a delay is possible for the high alarm (only in Europe for now),
- the Dexcom G7 (as the only CGM) has an official FDA approval for use in pregnancy (i.e., including gestational diabetes),
- the approved place to wear the sensor oddly differs between children and adults, as well as between Europe and America:
- Europe:
- adults: abdomen and upper arm,
- children: abdomen and upper buttock,
- America:
- adults: upper arm only,
- children: abdomen, upper arm and upper buttock.
- Europe:
When and where will Dexcom G7 be available?
The Dexcom G7 already had a CE label as of March 2022 and is available in UK, Ireland, Germany, Austria and Hong Kong.
Further rollout in Europe is planned, but it is still unclear which countries are first.
As of 8-12-2022, the Dexcom G7 also has an FDA label.
In America, the rollout is expected "in early 2023." There, too, it is unclear when and where Dexcom G7 will be available, but it is said to be "moving faster" than in Europe.
Although previously said to be cheaper to make than the Dexcom G6, the Dexcom G7 seems to be sold at the same price as the Dexcom G6.
What can we expect at Dexcom in 2023?
For the Dexcom G7, of course, we especially hope that it will finally be available in more countries, both in Europe and America.
Furthermore, for the Dexcom G7 in 2023, we also expect:
- the long-awaited integration into Tandem Control IQ (expected in mid-2023) and then into Omnipod 5 ("shortly after"),
- the direct-to-watch functionality (eliminating the need to carry your cell phone to see your sensor data on your smartwatch),
- and possibly a 15-day lifespan as well (although this could be longer).
Dexcom ONE would also migrate in "the future" to the form of the Dexcom G7.
And there is also already talk of the Dexcom G8. Maybe in 2023 we will find out what it will look like?
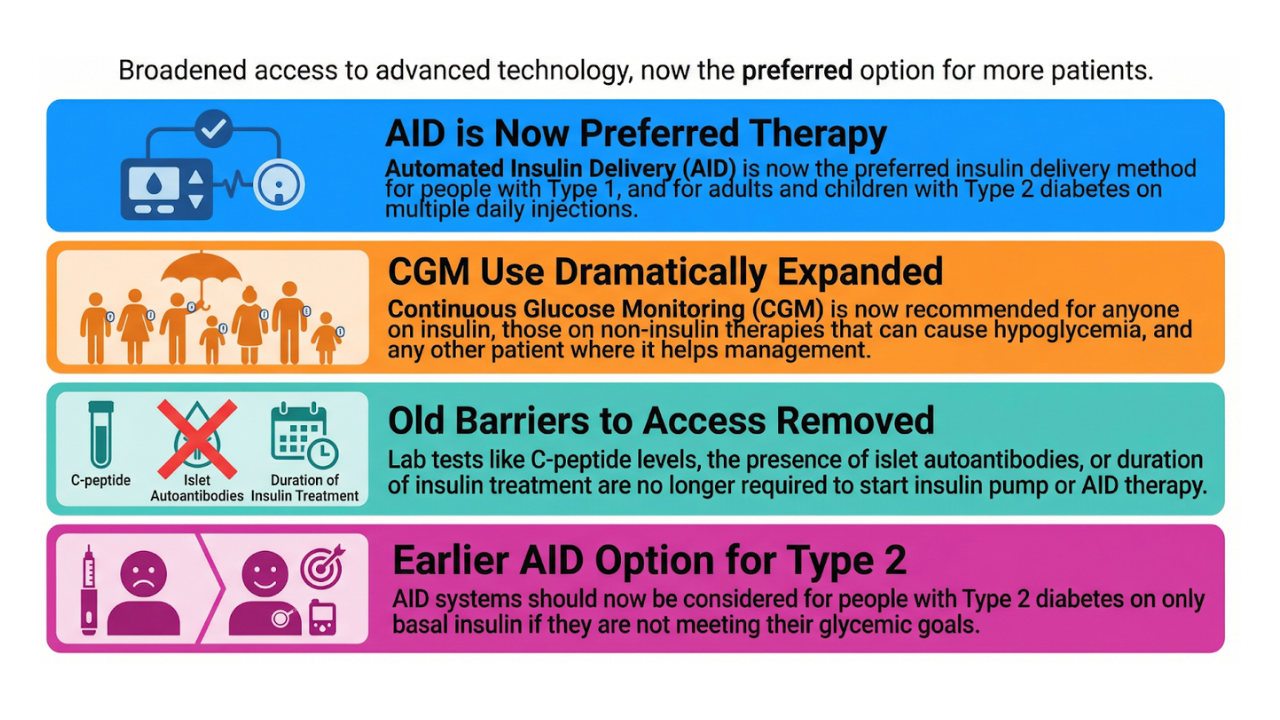
2. News from ADA Standards of Care 2023
Each year, the American Diabetes Association publishes the Standard of Care in Diabetes.
The 2023 version was published in Diabetes Care on 12-12-2022.
Here you can see the main guidelines around diabetes technology:
Continuous Glucose Monitor (CGM)
- 7.11 CGM should be offered to adults with diabetes using multiple daily injections or insulin pumps.
- 7.12 CGM should be offered to adults with diabetes on basic insulin *NEW*.
- 7.13 CGM should be offered to adolescents with type 1 diabetes who use multiple daily injections or insulin pumps.
- 7.14 CGM should be offered to youth with type 2 diabetes who receive multiple daily injections or insulin pumps.
- 7.19 CGM users should be educated about potential interfering substances and other factors that may affect accuracy *NEW*
Automated Insulin Delivery systems (AID)
- 7.24 Automated insulin delivery systems should be offered for youth and adults with type 1 diabetes and other types of insulin-deficient diabetes
- 7.25 Insulin pump therapy with or without sensor-augmented pump (stop-before-low) should be offered for youth and adults with type 1 diabetes and other types of insulin-deficient diabetes who are not able to use or do not choose an AID system
- 7.26 Insulin pump therapy can be offered to youth and adults on multiple daily injections with type 2 diabetes
- 7.28 Individuals with diabetes may be using systems not approved by the FDA, such as do-it-yourself closed-loop systems and others; healthcare professionals cannot prescribe these systems but should assist in diabetes management to ensure the safety of people with diabetes. *NEW*
- 7.29 Systems that combine technology and online coaching can be beneficial in treating prediabetes and diabetes for some individuals.
- 7.30 People with diabetes who are competent to safely use diabetes devices such as insulin pumps and continuous glucose monitoring systems should be supported to continue using them in an inpatient setting or during outpatient procedures, once competency is established and proper supervision is available. *NEW*
*NEW* CGM "should be offered" to adults with diabetes on (basal) insulin only
Following the recently published studies around the effect of CGM on the HbA1c of people who used basal insulin only (e.g. MOBILE study), the ADA updated its advice for this population. The recommendation for CGM in adults with diabetes on basal insulin only was updated from "can be used" to "should be offered."
There are already countries implementing this and reimbursing CGM for people with diabetes on basal insulin only, e.g.
- Dexcom G6 and Libre in Japan,
- and possibly soon in US cfr proposed Medicare reimbursement.
For people with diabetes who also use short-acting insulin, the advice remained: that they should also be offered CGM regardless of their type of diabetes.
*NEW* CGM users should be educated about possible interfering substances and other factors that may affect accuracy
ADA placed additional emphasis this year on the necessary education around substances that can lead to false sensor readings. They provided the following overview:
That the sensor glycemia on the Guardian sensors could be false high when consuming alcohol, I did not know.
So when in doubt, it's best to do a finger prick!
*NEW* People with diabetes can use systems not approved by the FDA, such as open-source closed-loop systems and others; health care providers cannot prescribe them but should assist in diabetes management to ensure the safety of people with diabetes.
Nice to see the ADA also taking a positive stance around the increasing use of open-source closed-loop systems.
The text goes into a little more detail about the role of the healthcare provider:
- they should ensure that people using an open-source closed-loop system have a backup plan for in case of pump failure,
- and they should evaluate and adjust the settings of the open-source closed-loop system (basal insulin delivery, carbohydrate ratio, correction factor, and insulin activity) as needed based on the individual's insulin need.
*NEW* People with diabetes who are competent to safely use diabetes devices such as insulin pumps and continuous glucose monitoring systems should be supported to continue using them in an inpatient setting or during outpatient procedures, once competency is established and proper supervision is available.
This guideline demonstrates the importance of letting people continue to use their devices during admission, if they are well enough to do so and have their supplies with them.
People who are used to managing their own glycemia will often be able to do this better than the nurses on the ward.
This would be best in accordance with hospital policy, though, and there would also be best some form of supervision, to be sure that glycemic control is reasonable.
From "guidelines about" to "more access to" diabetes technology
The ADA is clearly evolving along with diabetes technology and paving the way to facilitate implementation.
Of course, guidelines are 1 thing, and access is often another.
This is also clearly a concern of the ADA, cfr this interview with Dr. Bob Gabbay:
"I think the work that we all need to do collectively is to ensure that more people actually have access [to CGM]. One step is us making the recommendations.
The next big step is having this in the hands of the payers, ensuring access and removing some of the barriers that can be all sorts but from the provider side [...]
We need to make it simpler or easier for people to access."
Dr Bob Gabbay (Chief Scientific and Medical Officer for the American Diabetes Association)
3. International consensus on use of CGM in clinical trials
An international consensus on the proper use of CGM was published on 6-12-2022. You can read the article for free here.
Simultaneously with the publication, an ATTD online first video was also published, which you can watch for free on the ATTD educational platform.
You can see from the authors that this document is widely supported.
In doing so, this document was also signed by just about every scientific diabetes association (AACE, ADA, ADCES, DiabetesInda, EASD, ISPAD, JDS and JDRF).
Inclusion of CGM data in clinical trials will give us more information
The main goal of this consensus is to propose a standardized approach to the use of CGM data in clinical trials.
This will improve the use and interpretability of CGM data and give us useful information - beyond HbA1c - about treatments,
especially regarding hypoglycemia, postprandial hyperglycemia and glycemic variability.
Key recommendations at a glance
There were 23 recommendations. I show here some of the most important ones:
- Primary endpoints in CGM use in clinical trials:
- Time In Range (TIR) 70-180 mg/dl (3.9-10 mmol/l),
- Time Below Range (TBR) <70 mg/dl (<3.9 mmol/l) and <54 mg/dl (<3.0 mmol/l),
- Time Above Range (TAR) >180 (>10 mmol/l) ánd >250 mg/dl (>13.9 mmol/l).
- Coefficient of variation (CV) and standard deviation (SD)
- Mean glucose
- Secondary endpoints in CGM use in clinical trials:
- Time In Tight Range (TITR) 70-140 mg/dl (3.9-7.8 mmol/l) *NEW*
- Change in Glucose Management Indicator (GMI) *NEW*
- Extended hypoglycemic event rate <70 mg/dl (<3.9 mmol/l) *NEW*
- Extended hyperglycemic event rate >250 mg/dl (>13.9 mmol/l) *NEW*
- (Composite endpoints)
- A difference in TIR of >or= 5% may be considered clinically significant for an individual in a clinical trial.
- A difference in TI(T)R of 3% between 2 treatment groups may be considered clinically significant.
- In a clinical trial, CGM should be worn for a minimum of 14 days every 3 months.
- All CGM data should be reported, as well as data quality (how many people had >70% CGM data).
Time In Tight Range
This consensus used the term Time in Tight Range for the first time, which is glycemia between 70 and 140 mg/dl (3.9-7.8 mmol/l).
Thanks in part to closed-loop systems, many people with diabetes are already pursuing this tighter glycemic control today.
By defining this stricter glycemic control, we finally have tools to better compare the effects of certain closed-loop systems in the future.
A 3% difference in TITR between 2 treatment groups is considered clinically important, and it was suggested that studies be "powered" so that a 3% difference in mean TI(T)R can be detected.
What will be the role of HbA1c?
These consensus guidelines underscore that HbA1c is no longer sufficient to assess glycemic control.
Indeed, HbA1c says nothing about the TIR, postprandial hyperglycemia, number of hypos and glycemic variability.
The "30-year-old" HbA1c can be replaced by the GMI, according to Prof. Tadej Battelino, which you can find on the CGM curves.
The change in GMI is now also listed as a secondary endpoint for interpretation of CGM data.
Extended hypo/hyperglycemic event rate
This consensus also provides a way to start counting hypo/hyperglycemia events.
The definition of prolonged hypo/hyperglycemia is new here.
Thus, a distinction is now made between common and prolonged events of hypo/hyperglycemia:
- The common events of hypo/hyperglycemia are defined as:
- hypoglycemia (level 1): glycemia of 54-69 mg/dl (3.0-3.9 mmol/l) for >or= 15 minutes
- clinically significant hypoglycemia (level 2): glycemia of <54 mg/dl (<3.0 mmol/l) for >or= 15 minutes
- high glycemia (level 1): glycemia of 181-250 mg/dl (>13.9 mmol/l) for >or= 15 minutes
- very high glycemia (level 2): glycemia of >250 mg/dl (>13.9 mmol/l) for >or= 15 minutes
- Prolonged events of hypo/hyperglycemia are defined as:
- glycemia of <70 mg/dl (<3.9 mmol/l) for at least 120 minutes, event ends when glycemia is <or= 70 mg/dl (<or= 3.9 mmol/l) for >or= 15 minutes
- glycemia of >250 mg/dl (>13.9 mmol/l) for at least 90 minutes within one 120-minute period
On the one hand, it was noted that with CGM use, 3-6x more hypoglycemic events are detected than with the use of finger pricks alone,
but on the other hand, all these (level 1) hypoglycemic events may not be so relevant.
It is therefore suggested that participant-related outcomes should also be considered to better capture the clinical importance of hypoglycemia.
Interfering substances in CGM
The consensus also showed a list of possible substances that could lead to false sensor data.
This is largely similar to the list in the ADA guidelines, only here details are also shown for the Dexcom G4, G5 and Guardian 3 and 4.
Regarding the Guardian 3 and 4, there do seem to be some inaccuracies in the table, as there are normally no differences in terms of interfering substances between Guardian 3 and 4 (?).
Future for these guidelines
This year, a the consensus group will meet again for the ATTD in Berlin.
One of the issues that will be looked at is the definition of CGM guidelines for people without diabetes and/or prediabetes.
There was also a comment that sometimes there are people in whom the TIR is not sufficient to evaluate glycemic control, for example in certain races who typically have high postprandial hyperglycemia but a good TIR. At the next ATTD, we would get more data on certain ethnic glycemia profiles.
Looking forward to it :-)
4. Tandem bought Swiss Sigi pump
On 13-12-2022, Tandem announced that they have purchased Swiss AMF Medical for $216 million.
AMF Medical developed the Sigi insulin pump. This phone-controlled insulin patch pump is unique because of
- the use of pre-filled insulin PumpCarts (which until now has only been used in cathter pumps),
- the emphasis on ease of use,
- and the use of a patented "bubble-free" pump technology with "highly accurate" insulin delivery and "rapid" occlusion detection.
It is said to be smaller than the Omnipod, Eopatch and AccuCheck Solo insulin pumps.
AMF Medical calls their pump the "Nespresso" of insulin pumps.
Tandem hopes to bring the Sigi insulin pump to market by about 2027, so first the Mobi pump is still planned.
So the launch of new devices at Tandem will look something like this - each time integrating the Control IQ algorithm:
- Mobi semi-patch pump (submitted to FDA 2022, launch 2023?)
- t:slim X3 catheter pump
- Mobi: tubeless patch pump
- Sigi patch pump (2027)
So great prospects!
5. Lilly will not distribute YpsoPump in US

As a final little surprise, Lilly will not be distributing the YpsoPump in US after all.
- Ypsomed will still submit the YpsoPump for an FDA label in 2023, though. Commercialization in US will thus be done by another partner.
- Lilly will continue to focus on their current portfolio including Trulicity® and the not-to-be-underestimated Moujaro® (tirzepatide).
And so everything is constantly moving....
As we enter the new year, it's important to make sure you're up to date on the latest news and updates in diabetes technology.
We've done the work for you and collected all the major news stories from December, so you'll be fully informed before you enter 2023.
From FDA approvals to new guidelines to shifts in closed-loop system providers, staying abreast of these changes is important for anyone working in or living with diabetes.
Looking for an overview of all diabetes technology available in 2023?
Look no further and download it here:
> Click here for the Diabetes Technology 2023 Overview for people with diabetes
> Click here for the Diabetes Technology 2023 Overview for healthcare providers
Good luck and happy new year!